CARDIOVASCULAR JOURNAL OF AFRICA • Volume 25, No 6, November/December 2014
e8
AFRICA
Under general anaesthesia, after pealing back the pleura, the
pericardium was reached via an incision in the fifth
intercostal
space by left anterior thoracotomy. The pericardium was
opened from the anterolateral site and the left ventricle was
explored. The Medtronic single coil (model 6937; Medtronic Inc,
Minneapolis, MN) electrode was fashioned as a halo and secured
with non-absorbable suture material. This halo was placed
between the inferior surface of the heart and the diaphragmatic
surface of the pericardium. Through the same incision an
active fixation bipolar epicardial lead (model 4968; Medtronic
Inc, Minneapolis, MN) was fixed to the lateral wall of the left
ventricular epicardium in a position where sensing, pacing
and impedance measurements were satisfactory. Ventricular
fibrillation (VF) was induced with ‘shock-on-T’ and the therapy
was successful in defibrillating VF at 25 J (a 10-J safety margin).
Both leads were then tunnelled through the subcutaneous
tissue to be placed inside a generator pocket created in the left
sub-pectoral region.
As soon as bleeding was controlled, the layers were closed in
the anatomical positions. There were no complications in the peri-
operative or postoperative periods. The patient was discharged
on medical treatment: acetylsalicylic acid, angiotension
converting enzyme inhibitor, beta-blocker, aldosterone receptor
antagonist and furosemide. During the eight-month follow up,
two appropriate shocks were delivered.
Discussion
The Fontan operation has been the primary surgical technique
used for palliation of patients with single-ventricle physiology.
5
It is based on leading systemic venous blood into the pulmonary
circulation and pumping pulmonary venous blood into the
systemic circulation by a unique functional ventricle.
Arrhythmias are frequently observed and are associated with
morbidity and mortality in Fontan patients. It is reported that
the frequency of arrhythmias gradually increases, and reaches
50% by 20 years of follow up.
2,3
Postoperative early arrhythmias
are a result of trauma to the sinus node and sinus node artery.
6,7
In the late period they may develop due to atrial dilatation and
distension,
2,7
and surgical scars.
Major clinical studies investigating late arrhythmias in Fontan
patients are summarised in Table 1.
2,8-15
Intra-atrial re-entrant
tachycardia and sinus bradycardia are seen most commonly;
ventricular arrhythmias are more rare and these arrhythmias
arise from surgical scars. In a multicentre, cross-sectional study,
16
ventricular tachyarrhythmia was reported in 18 (3.5%) of 520
patients in whom a Fontan procedure had been performed.
Nakamura and collegues
13
retrospectively reviewed 48 patients
who survived and were followed up for more than 15 years,
among 110 patients who underwent a Fontan operation. Fifteen
years after the Fontan operation, six patients (12.5%) with a
higher age at operation developed VT, irrespective of ventricular
function. The interval between the Fontan operation and onset
of VT correlated inversely with age at Fontan operation. They
suspected that pathological changes caused by longstanding
cyanosis and volume overload before the Fontan operation may
have produced arrhythmogenic areas, resulting in VT, with an
additional postoperative factor, age itself, in patients when they
got close to their thirties.
In our case, the patient had undergone the Fontan operation
14 years earlier when she was 30 years old. Her left ventricular
ejection fraction was also quite low. These factors may have
played a role in the development of VT in our patient.
For structural reasons, it may be difficult to implant either
a pacemaker or an ICD in patients with congenital heart
disease,
7,17
especially those in whom a Fontan procedure had
been performed. In conditions where access to the right ventricle
from the venous system is anatomically impossible (e.g. tricuspid
atresia), or there is no functional right ventricle (e.g. double-
inlet left ventricle), device implantation can be performed with
alternative methods other than the conventional transvenous
approach.
An earlier solution was the placement of epicardial patch
electrodes and pacing/sensing leads. The epicardial patch
technique has been associated with post-pericardiotomy
syndrome, mediastinitis and constrictive pericarditis.
18
Non-traditional alternative surgical methods include video-
assisted thoracoscopy, a subxiphoid approach or lateral
thoracotomy for placemant of either an epicardial coil and/
or ventricular pace-sense leads.
19
In patients with Fontan,
although small in number, there are cases in whom an epicardial
pacemaker/ICD has been implanted.
In a retrospective study by Cannon
et al
.,
20
eight patients with
non-traditional lead placement were identified and included.
Four of them had undergone previous Fontan operations because
of double-inlet left ventricle or tricuspid atresia. The indications
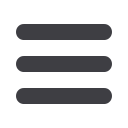
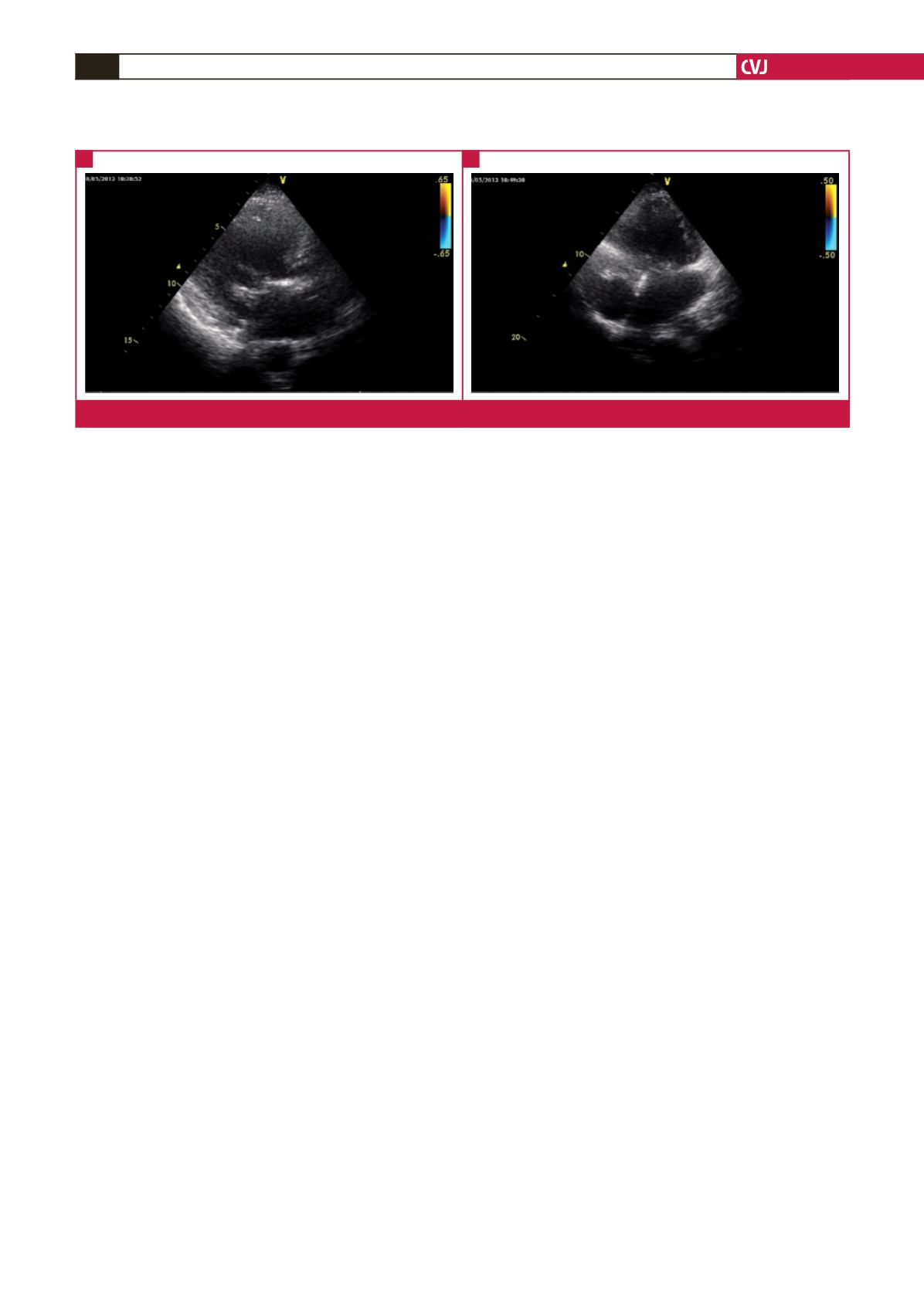
Fig. 4.
Transthoracic echocardiographic images in the parasternal long-axis and apical four-chamber views.
A
B



















