
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 1, January/February 2015
AFRICA
35
hundred and thirteen (213) patients were evaluated; 118 patients
(139 limbs) had had stents placed and 95 (104 limbs) had had
bypass surgery. We did not include patients who had had balloon
angioplasty alone.
Most of the patients (60%) presented with critical limb
ischaemia and the remainder with crippling claudication.
Among the patients with critical limb ischaemia, 40% presented
with rest pain and the remainder with tissue necrosis (20%). Both
treatment groups had similar risk factors. Follow up comprised
clinical review at one month, six months and yearly thereafter.
Stent treatment group
Due to the demand for minimally invasive procedures by
patients, and the frequent presence of multiple co-morbidities
in poor operative-risk patients, our practice has focused on
an endovascular-first approach for most of the patients with
less extensive lesions [TASC (Trans-Atlantic Inter-Society
Consensus) IIA and B], reserving open surgical bypass for
patients who had more extensive lesions (TASC IIC and D) or
femoral artery origin disease.
All stenting was performed in a hybrid endovascular operating
theatre with fixed imaging capabilities. In most cases, ipsilateral
antegrade access was obtained with a 6-F sheath by percutaneous
groin puncture. Distal run-off vessels were evaluated before
crossing the lesions. All patients were given intravenous heparin
(80 IU/kg).
Accurate measurement of lesion length and vessel diameter
was obtained by calibration techniques. Lesions were crossed
with a hydrophilic guide wire and an angled, tapered catheter,
and the sub-intimal technique was used in some of the complete
occlusive lesions.
All patients received a self-expanding uncovered nitinol stent
from different manufacturers. More than one stent was used in
some patients. All stents were ballooned post deployment. Post
stent procedures, all patients received a loading dose of 300 mg
of clopidogrel followed by 75 mg daily for four weeks, and were
given aspirin and statin therapy on a long-term basis.
Bypass treatment group
Most bypasses were from the common femoral artery to
above-the-knee popliteal artery, using polytetrafluoroethylene
(PTFE) grafts. Reversed autogenous saphenous vein grafts
were used when a suitable vein was available. All bypass grafts
had a distaflo cuff configuration with ring reinforcement. Post
operatively, all patients continued with aspirin and statin therapy
on a long-term basis.
Statistical analysis
In the case of quantitative data, means and 95% confidence
intervals (95% CI) were reported around sample estimates.
Fisher’s exact test (two-tailed) and the
t
-test (two-tailed) were
used for differences in proportions. A
p
-value of
≤
0.05 was
considered significant.
Results
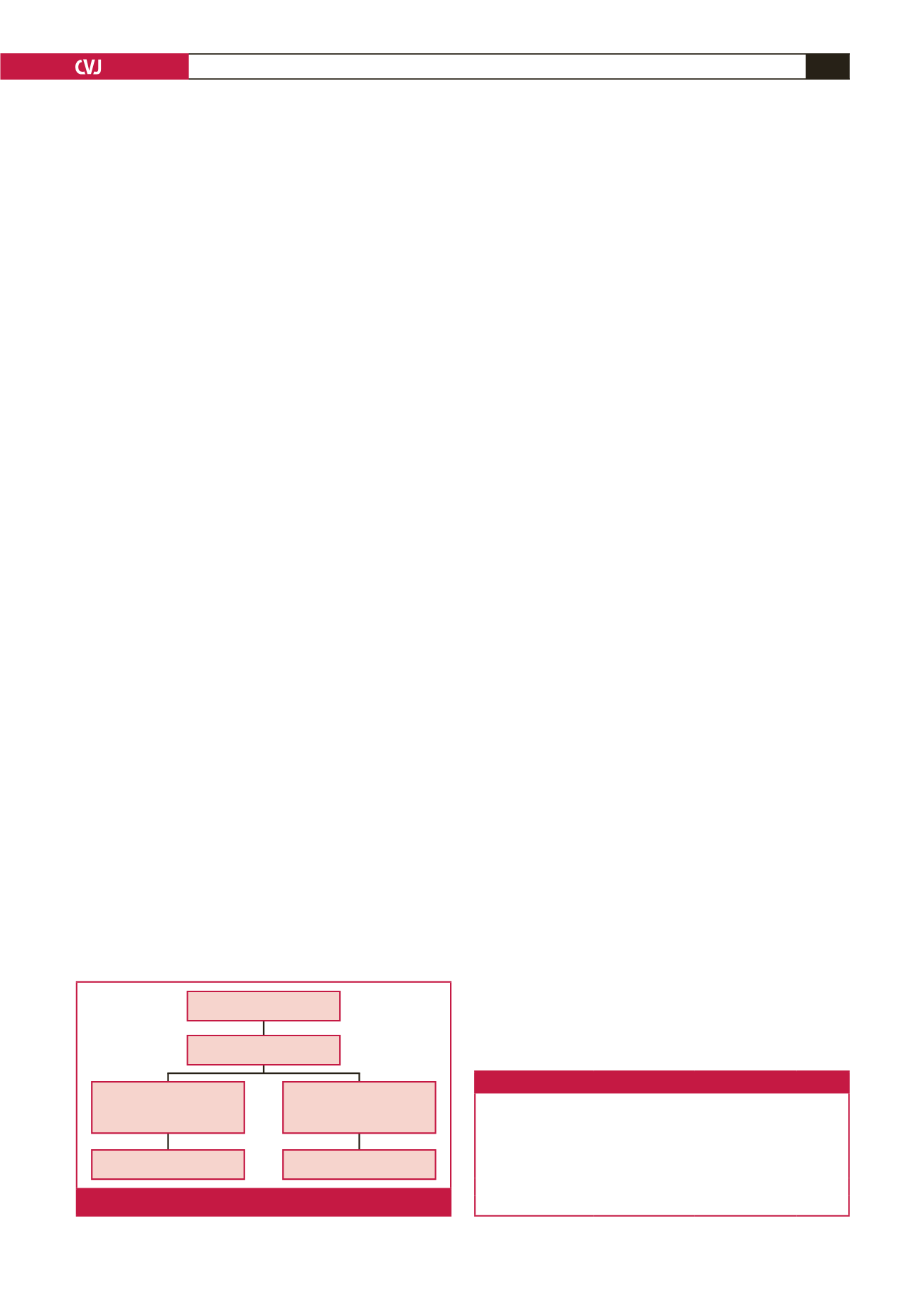
Two hundred and forty-three limbs were treated in 213 patients.
Stenting was done in 139 limbs (57%) and bypass in 104 limbs
(43%) (Fig. 1). The average age of the patients was 66 years
(95% CI: 64.66–67.17), 73% were male and the male-to-female
ratio was 2.73. The average age was similar in both treatment
groups: 67 years (95% CI: 65.01–68.75) in the stent group and
65 years (95% CI: 63.17–66.27) in the bypass group (
p
=
0.08).
The stent group had a similar gender distribution compared to
the whole group (69% male and 31% female), whereas the bypass
group had more males (79%), however this difference was not
statistically significant (
p
=
0.11).
Critical limb ischaemia (CLI) was the presenting symptom in
the majority of patients [128 (60%)]. Of these, 86 patients (40%)
presented with rest pain and 42 (20%) with tissue necrosis or
gangrene. The remainder of the patients presented with severe
claudication [85 (40%)]. The distribution of severe claudication
and critical limb ischaemia was similar in both treatment groups
(Table 1), except that more patients presented with tissue necrosis
in the stent group (26%) compared with the bypass group (12%)
(
p
=
0.009).
The prevalence of cardiovascular risk factors, for example
hypertension, smoking, ischaemic heart disease (IHD),
cerebrovascular disease (CVD), and renal failure was similar
across the treatment groups, except for diabetes mellitus, which
was higher in the stent group (51 vs 37%,
p
=
0.05), as
shown in Table 2. The presentations according to the TASC II
classification are shown in Table 3. Overall, 80% of TASC A
and TASC B lesions received stents and 76% of TASC C and
D lesions received bypass (
p
=
0.0001). In the stent group 26%
of patients had adjunctive procedures, compared to 16% in the
bypass group (
p
=
0.138) (Table 4).
During the one-year follow-up period there were 30 stent
occlusions (22%). They were treated by balloon angioplasty
alone (three patients), re-stenting (11), femoro-popliteal bypass
(13), and three patients were treated conservatively. In the bypass
group 18 patients had graft occlusions (17%) and they were
Stenting
118 (139)
57%
Bypass
95 (104)
43%
243 limbs
213 patients
Fig. 1.
Total patients and procedures.
Table 1. Clinical presentation
Stent
n
(%)
Bypass
n
(%)
p
-value
Severe claudication
42 (36)
43 (45)
0.16
Rest pain
45 (38)
41 (43)
0.48
Tissue necrosis
31 (26)
11 (12)
0.009
Total
118 (100)
95 (100)
Percentage rounded to the nearest integer.



















