
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 2, March/April 2015
AFRICA
87
of 3.5 mmol/l. Her father had died of a myocardial infarct aged
65 years. Her blood pressure was 120/75 mmHg. No clinical or
electrocardiographic abnormality was detected.
She went mountain biking on the day of her presentation. She
described the sudden onset of left-sided chest pain radiating to
the left side of her neck, shoulder and arm, starting immediately
after she had crested a hill. The pain was still present when she
arrived in the emergency room 90 minutes later.
The clinical examination was unremarkable. Her pulse rate
was 80 beats/min and her blood pressure was 111/71 mmHg.
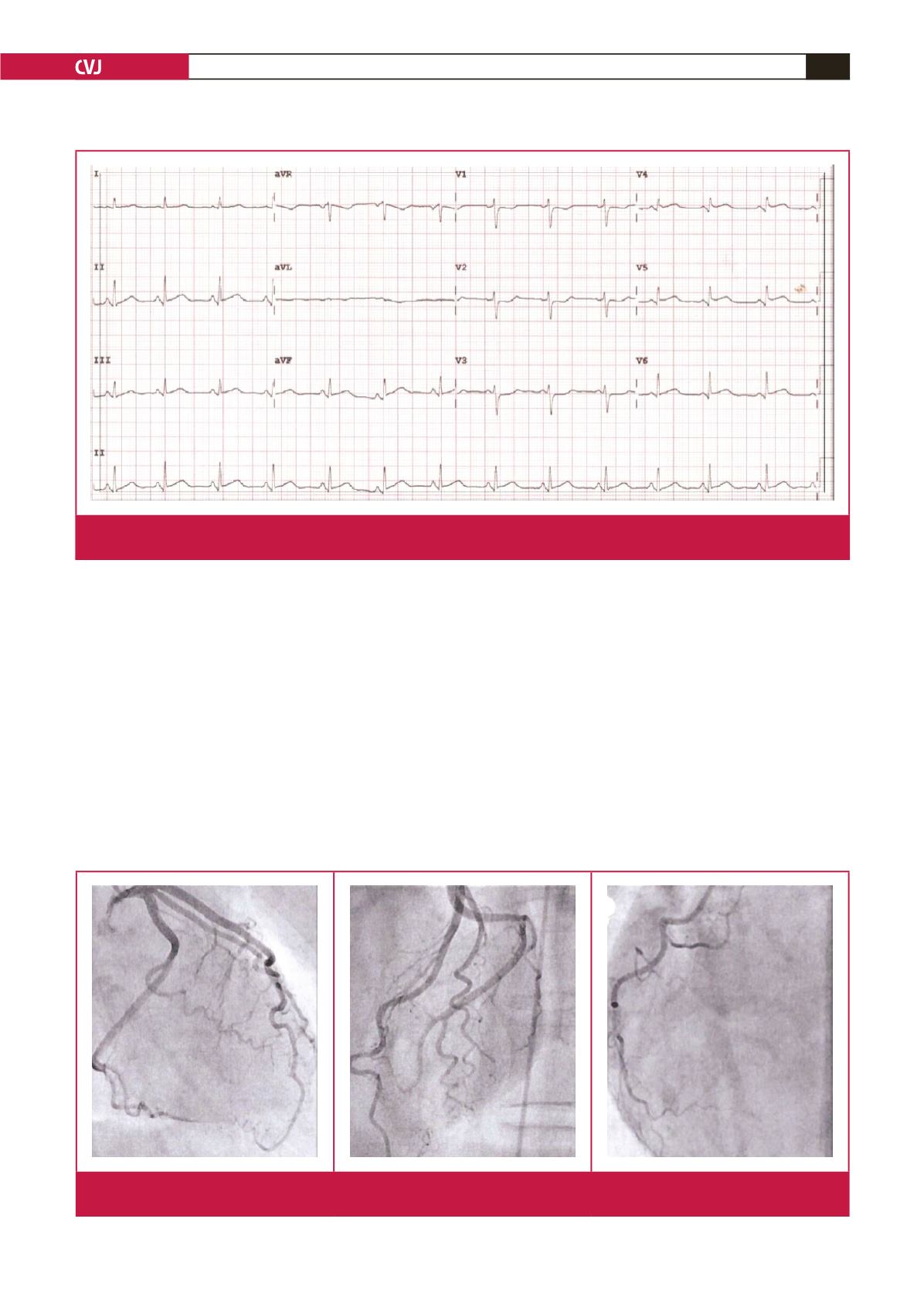
The resting electrocardiogram showed ST-segment elevation of
1–2 mm in S2, S3, aVF and V4–6 with ST-segment sag in V1–
V3 (Fig. 2), consistent with a diagnosis of acute posterolateral
myocardial infarction. She was treated with aspirin, clopidogrel
and enoxaparin and immediately thereafter transferred to the
cardiac catheterisation laboratory for coronary angiography.
The left ventriculogram showed minor hypokinesia of the
inferior wall. Her coronary arteries were considered to be patent
with good distal run-off (Fig. 3). Her hs-troponin T had been 29
ng/l when she presented and rose to 351 ng/l over the next 150
minutes. Conservative medical treatment was continued and the
patient was admitted to the coronary care unit where she ran an
uneventful course.
She left hospital on day three on beta-blockade and dual
antiplatelet therapy intended to be continued for 12 months.
She was advised to discontinue hormone replacement therapy.
She has remained asymptomatic in the two months since her
discharge.
Fig. 2.
The electrocardiogram obtained on admission, showing inferolateral ST-segment elevation and ST-segment depression in
the anterior leads.
Fig. 3.
The coronary angiogram obtained on admission. Left coronary artery in right anterior oblique and left anterior oblique projec-
tions and right coronary artery in left anterior oblique projection.

















