
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 2, March/April 2015
e4
AFRICA
tender by deep palpation and 8 cm larger in circumference than
the right calf.
There was no blood pressure difference between the lower
limbs and the ankle–brachial indices (ABI) were similar in both
limbs. The posterior tibial and dorsalis pedis pulses were normal,
and the deep tendon reflexes, strength and sensation were all
normal.
Cardiac, chest and abdominal examinations were within
normal limits. Head, neck and upper extremity examinations
were unremarkable.
Laboratory investigations revealed a haemoglobin of 12.4
g/dl, granulocyte count of 10 650 cells/mm
3
and platelet count
of 428 000 cells/mm
3
. His prothrombin time was 13 seconds,
activated prothromboplastin time was 29.3 seconds, and
international normalised ratio was 1. Biochemical analyses were
within normal levels.
The patient underwent abdominal and Doppler
ultrasonography (DUSG) for evaluating the lower extremity
venous system. Abdominal ultrasonography was normal and
DUSG revealed a mildly enlarged left external iliac vein, but
the proximal main iliac vein was entrapped at the level of the
crossing with the left iliac artery. It did not show any thrombosis
of the veins of the lower limbs.
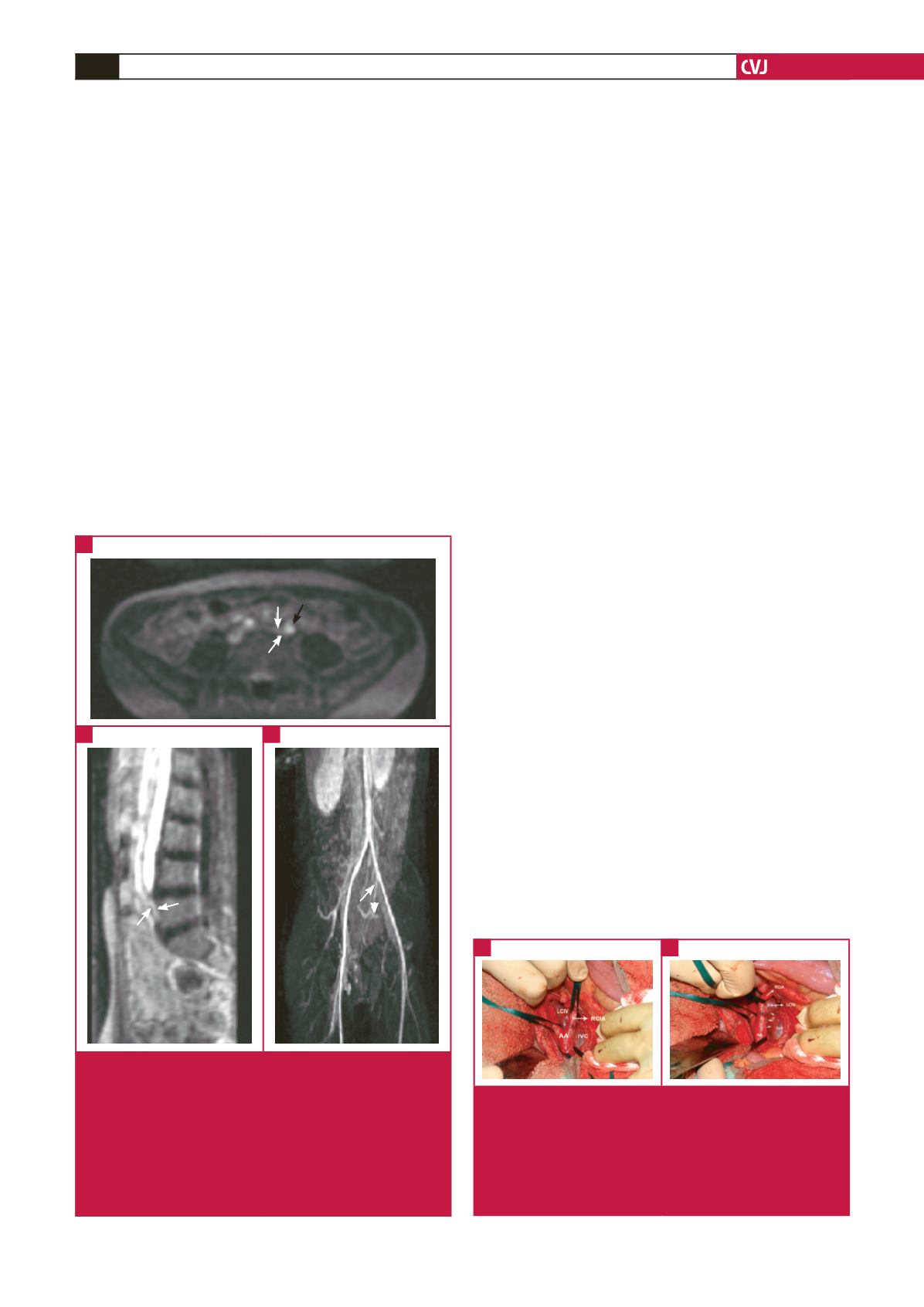
An iliac MR venography (MRV) was performed with
two-phase contrast injection, of which the second injection was
just four minutes after the first, to obtain images of arterial
and venous vessels in the same slice. The MRV images showed
compression of the left proximal iliac vein between the vertebra
and the left iliac artery (Fig. 2). The venous system caudal to the
obstruction was dilated (Fig. 2C).
The patient’s physical examination and imaging findings
were diagnostic of an atypical presentation of MTS. Surgical
intervention was planned after consultation with the
cardiovascular surgery department.
The operation was performed under general anaesthesia via
a median laparotomy incision. The abdominal aorta, bilateral
common iliac arteries, inferior vena cava, and left and right
common iliac veins were dissected carefully. The left common
iliac vein was found to be connected to the postero-inferior part
of the inferior vena cava, and it was compressed between the
right common iliac artery and columna vertebralis (Fig. 3A, B),
which was inconsistent with the radiological findings.
The left common iliac vein was fragile and enlarged, and there
were enlarged collateral veins at the posterior part of the left
common iliac vein, which made complete dissection of the vein
impossible. Therefore reconstruction of the left common iliac
vein from the bifurcations to the inferior vena cava was thought
to be impossible. The surgeons decided to make an interposition
of the great saphenous vein graft between the left common iliac
vein and the inferior vena cava (Fig. 4).
The postoperative period was uneventful. In order to prevent
early-term thrombosis of the saphenous vein graft, we used
standard heparin (1 cm
3
intravenous per six hours daily, for four
days). The swelling of the extremity gradually decreased and
resolved.
Discussion
Although the usual manifestation of MTS is compression of
the left common iliac vein by the right common iliac artery,
compression of the left common iliac vein by the left internal iliac
artery and left common iliac artery has also been reported.
5,6
Our
case showed an unusual manifestation of MTS on radiological
Fig. 3.
Pre-operative images. A: Connection of the left
common iliac vein to the postero-inferior part of the
inferior vena cava. B: The left common iliac vein was
pressed between the right common iliac artery and
the columna vertebralis. LCIV, left common iliac vein;
RCIV, right common iliac vein; AA, abdominal aorta;
IVC, inferior vena cava.
A
B
Fig. 2.
A: Axial-plain MR angiography image showed left
iliac vein compression (white arrows) by the left iliac
artery (black arrow). B: Sagittal-plain reconstructed
MR angiography image showed a markedly narrowed
left iliac vein (white arrow). C: Oblique coronal-plain
MIP (maximum intensity projection) image revealed
venous compression while crossing the left iliac artery
(white arrow) and dilated caudal segment iliac veins
(arrow head).
A
B
C

















