
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 3, May/June 2015
e4
AFRICA
Case Report
Treatment of right ventricular perforation during
percutaneous coronary intervention
Guoqiang Gu, Jidong Zhang, Wei Cui
Abstract
Percutaneous coronary intervention (PCI) is widely used to
treat stenotic coronary arteries caused by coronary heart
disease. Coronary artery perforation is a rare but dreaded
complication of PCI. Here, we report the successful treatment
of a patient with coronary perforation of the right ventricular
cavity. To our knowledge, this is the first report of its kind.
The patient was a 69-year-old woman with intermittent
chest tightness and chest pain of about five years’ duration
who was hospitalised for severe chest tightness and pain
persisting for three days. She had a history of hypertension
and hyperlipidaemia; routine admission examination showed
no other abnormalities. Results of routine blood, urine and
stool tests, liver and kidney function, clotting time, electro-
cardiogram, chest radiography and echocardiography were
normal.
Although coil embolisation rather than balloon is safe
and effective for treating coronary artery perforation, it
may be not the best choice overall. If the perforation breaks
through into the right ventricle, we may just monitor closely
rather than treat. That course may be beneficial for patients
in that it reduces the risk of myocardial cell necrosis. This
case provides useful information for the treatment of such
patients in the future.
Keywords:
percutaneous coronary intervention (PCI), coronary
artery perforation, myocardial cell necrosis, right ventricle,
cardiac tamponade
Submitted 24/6/14, accepted 27/11/14
Cardiovasc J Afr
2015;
26
: e4–e6
www.cvja.co.zaDOI: 10.5830/CVJA-2014-072
Percutaneous coronary intervention (PCI) is a widely used
non-surgical procedure to treat stenotic coronary arteries caused
by coronary heart disease.
1,2
The benefit of PCI to the patient
is great, but the procedure is accompanied by risk. Coronary
artery perforation is a rare but dreaded complication of PCI,
with a reported incidence from 0.12–0.93% and a mortality rate
of about 7–41%.
3–14
In most cases, the perforation breaks through into the
pericardium, which may cause cardiac tamponade.
15
Coronary
perforation can also involve the cardiac chambers.
16
Here we
report the successful treatment of a patient with coronary
perforation of the right ventricular cavity and provide a brief
review of the literature on the treatment of coronary perforation
during PCI.
Case report
The patient was a 69-year-old woman with intermittent chest
tightness and chest pain over the previous five years. She
was hospitalised for severe chest tightness and chest pain
persisting for three days. She had a history of hypertension
and hyperlipidaemia; the admission examination showed no
other abnormalities. Routine blood, urine and stool tests, liver
and kidney function, clotting time, electrocardiogram, chest
radiography and echocardiography were normal. A diagnosis of
coronary artery disease was considered.
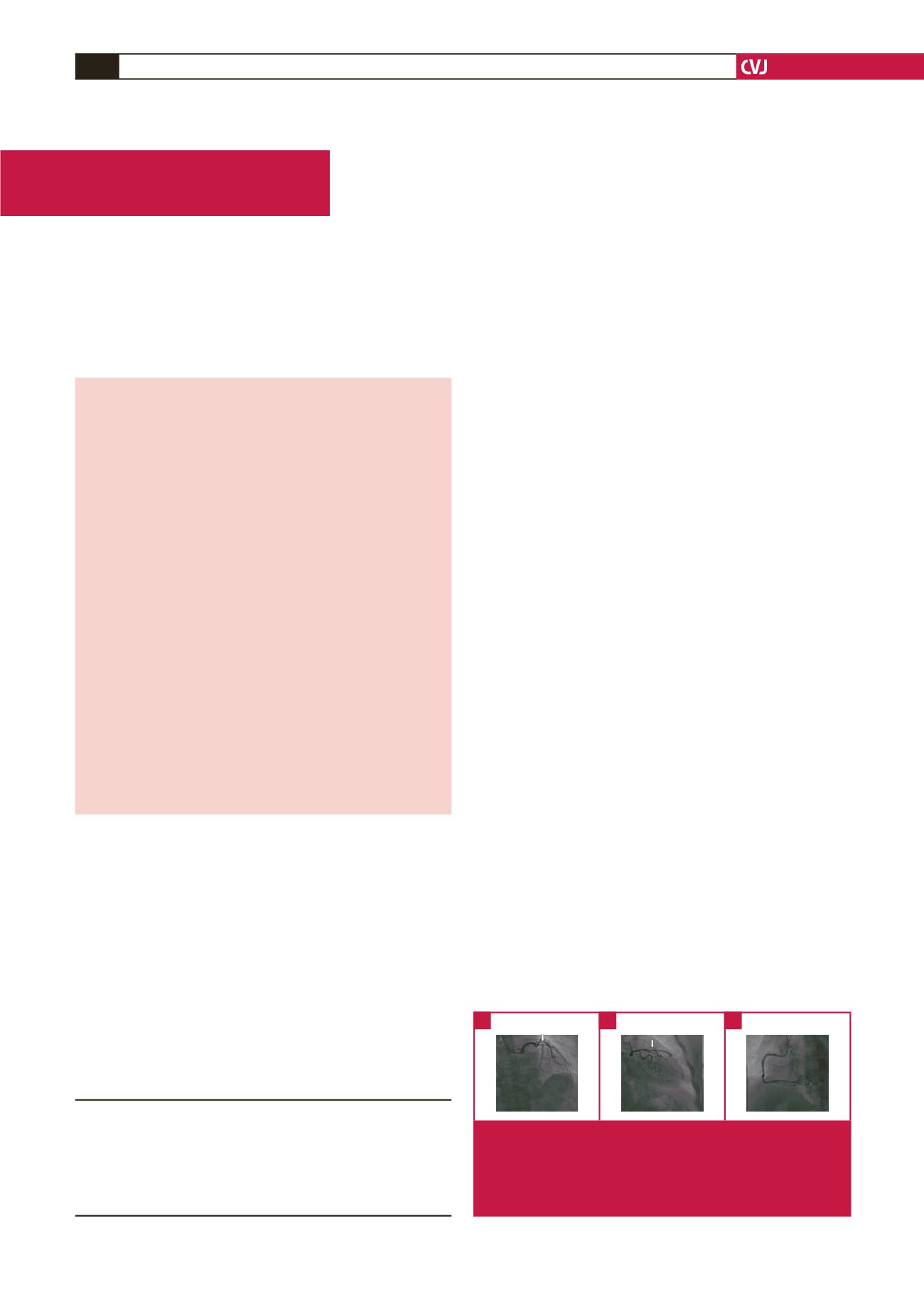
Coronary angiography showed a right coronary artery-
dominant circulation. The left main coronary artery was normal,
80% of the middle segment of the left anterior descending
(LAD) coronary artery showed stenosis, and the diagonal
branch issuing from the site of the stenosis was thicker than the
LAD artery. Plaques, but no obvious stenosis, were found in the
circumflex and right coronary arteries (Fig. 1A–C).
After discussing treatment with the patient, it was decided to
perform PCI of the LAD artery. Because of the narrow opening
of the diagonal branch, and because the diagonal branch was
thicker than the LAD artery, we planned to implant a stent at
Department of Cardiology, Hebei Institute of Cardiology,
Second Hospital of Hebei Medical University, Shijiazhuang,
Hebei, China
Guoqiang Gu, MD
Jidong Zhang, MD
Wei Cui, MD,
cuiwei21c@hotmail.comFig. 1.
(A) Stenosis is shown in 80% of the middle segment of
the LAD artery. (B) A diagonal branch issuing from the site of
stenosis is thicker than the LAD artery. (C) The circumflex and
the right coronary arteries showing visible plaques but no obvi-
ous stenosis.
A
B
C

















