
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 3, May/June 2016
146
AFRICA
statistical error that could have been introduced because of
disease severity and procedure differences.
In this study, fewer postoperative complications and lower
mortality rate were detected in the subclavian artery group
(Table 2). Undoubtedly, the lower incidence of neurological
dysfunction could be attributed to selective cerebral perfusion
through subclavian cannulation.
5
We also found that subclavian
artery cannulation provided better perfusion for other visceral
organs (Table 2).
Two possible hypotheses may elucidate why. First, according
to the Hagen–Poiseuille law,
6
the pressure drops in a fluid flowing
through a long cylindrical pipe. So under constant blood flow,
cardiac and sternal perfusion may not be adequate with femoral
cannulation, especially when the aorta is dissected. Inevitably,
sternitis and myocardial injury would be higher in the femoral
cannulation group. Second, we assume that subclavian cannulation
would pump major blood flow into the true lumen, while femoral
cannulation pumps more blood into the false lumen.
Based on our evaluation, femoral cannulation introducedmore
retrograde dissection and exacerbated perfusion of the visceral
organs. Survivors who underwent subclavian cannulation had
better recovery during the postoperative hospital course, which
might be attributed to better perfusion of the visceral organs.
In other words, subclavian rather than femoral cannulation
could achieve a lower incidence of visceral malperfusion during
surgeries for AADA.
Our univariate analysis of hospital mortality revealed many
risk factors, including pre-operative respiratory failure, peri-
operative CPB time
>
200 min, postoperative acidosis, troponin
I
>
2.0 ng/dl, and acute renal failure (Table 3). Myocardial
injury has been thought to be a risk factor during major aortic
surgery, particularly when the thoracic aorta is involved.
7-8
Although femoral cannulation was eliminated as a risk factor by
multivariate analysis, it seemed to have a trend towards increased
mortality because it resulted in a higher postoperative troponin
I level, which leads to increased peri-operative cardiac injury,
which reached statistical significance in the multivariate analysis.
The significance could be confirmed if more patients are enrolled
in the future.
This study has several limitations. First, the cohort was
relatively small, but despite this, we still identified an advantage
in subclavian cannulation, which suggests a significant benefit
for simple reconstruction of the ascending aorta. Second, the
data were collected from 2003 to 2010. Surgical techniques and
general postoperative care may have improved in the latter part of
the study, which could explain the unusually high mortality rate
of femoral cannulation in the earlier phase. Third, the study was
retrospective and not randomised. More prospective, randomised,
controlled trials should be designed to support our hypothesis.
Conclusion
Cardiac failure and visceral malperfusion are both fatal
complications of AADA surgery.
9,10
In Christian and co-workers’
study, antegrade perfusion to the true lumen appeared to
be associated with superior long-term survival after hospital
discharge.
11
Based on our evaluation, we believe subclavian
cannulation could provide better perfusion, not only for the
brain but also for the myocardium and other visceral organs,
leading to lower mortality rates and better recovery following
AADA procedures.
References
1. Gulbins H, Pritisanac A, Ennker J. Axillary versus femoral cannulation
for aortic surgery: enough evidence for a general recommendation?
Ann
Thorac Surg
2007;
83
:1219–1224.
2. Wong DR, Coselli JS, Palmero L,
et al.
Axillary artery cannulation in
surgery for acute or subacute ascending aortic dissections.
Ann Thorac
Surg
2010;
90
:731–737.
3. Neri E, Massetti M, Capannini G,
et al.
Axillary artery cannulation in
type A aortic dissection operations.
J Thorac Cardiovasc Surg
1999;
118
:
324–329.
4. Numata S, Ogino H, Sasaki H,
et al
. Total arch replacement using ante-
grade selective cerebral perfusion with right axillary artery perfusion.
Eur
J Cardiothorac Surg
2003;
23
: 771–775.
5. Zierer A, El-Sayed Ahmad A, Papadopoulos N,
et al
. Selective antegrade
cerebral perfusion and mild (28°C–30°C) systemic hypothermic circula-
tory arrest for aortic arch replacement: results from 1002 patients.
J
Thorac Cardiovasc Surg
2012;
144
: 1042–1049.
6. Pozrikidis C.
Fluid Dynamics: Theory, Computation, and Numerical
Simulation
, 2nd edn. New York, London: Springer Science, 2009: 362–383.
7. Hafez HM, Berwanger CS, McColl A,
et al
. Myocardial injury in major
aortic surgery.
J Vasc Surg
2000;
31
: 742–750.
8. Haggart PC, Adam DJ, Ludman PF, Bradbury AW. Comparison of
cardiac troponin I and creatine kinase ratios in the detection of myocar-
dial injury after aortic surgery.
Br J Surg
2001;
88
: 1196–1200.
9. Girdauskas E, Kuntze T, Borger MA,
et al
. Surgical risk of preoperative
malperfusion in acute type A aortic dissection.
J Thorac Cardiovasc Surg
2009;
138
: 1363–1369.
10. Deeb GM, Patel HJ, Williams DM. Treatment for malperfusion syndrome
in acute type A and B aortic dissection: a long-term analysis.
J Thorac
Cardiovasc Surg
2010;
140
(Suppl 6): S98–S100; discussion; S142–S146.
11. Christian DE, Konstantin VA, Jaqueline da RS,
et al
. Impact of perfu-
sion strategy on outcome after repair for acute type A aortic dissection.
Ann Thorac Surg
2014;
97
: 78–86.
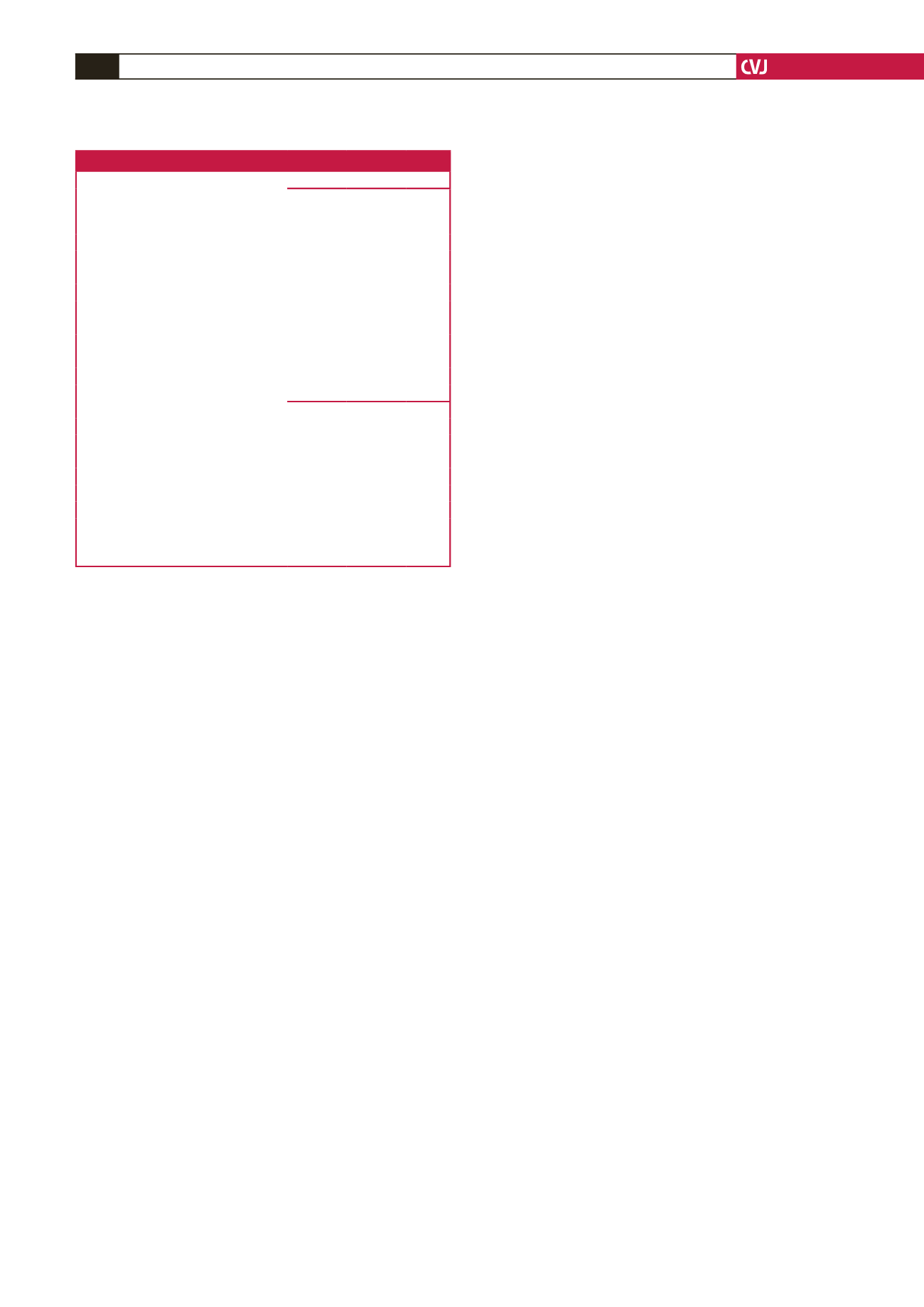
Table 3. Significant risk factors associated with hospital mortality
Univariate analysis
Survival
group
Mortality
group
p-
value
Variables
n
(%)
n
(%)
Total number
40 (100)
11 (100)
Pre-operative
Respiratory failure
2
6
<
0.001
Peri-operative
Cardiopulmonary bypass time
>
200 mins
10
9
<
0.001
Post-operative
pH
<
7.2
1
8
<
0.001
Troponin I
>
2.0 ng/dl
4
8
<
0.001
Acute renal failure
11
11
<
0.001
Multivariate analysis
Variables
OR 95% CI
p-
value
Pre-operative
Respiratory failure
12.84 1.48–111.0 0.020
Peri-operative
CPB time
>
200 min
13.49 1.29–140.1 0.029
Post-operative
pH
<
7.2
88.63 1.178–4.39 0.003
Troponin I
>
2.0
20.08 1.37–293.4 0.013
AR, aortic regurgitation; CRP, C-reactive protein; CI, confidence interval; OR,
odds ratio; CPB, cardiopulmonary bypass.

















