
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 3, May/June 2016
AFRICA
145
strokes in two. All five patients with neurological complications
survived and were released from hospital. One stroke patient died
of pneumonia with sepsis within three years. Twenty-six (51%)
patients required transfusions of more than 500 ml packed red
blood cells after surgery, and four (8%) underwent re-sternotomy
for haemostasis. Furthermore, 12 (23%) had pneumonia, five
(9%) had ARDS, and 22 (43%) developed acute renal failure.
The subclavian group showed a significantly lower incidence of
mediastinitis (
p
=
0.01), neurological dysfunction (
p
<
0.001), acute
renal failure (
p
=
0.03), and mortality (
p
=
0.04) (Table 2).
In the 24-hour postoperative biochemistry data (Table 2),
we found metabolic acidosis and hyperamylasaemia to be
significantly higher (
p
<
0.05) in the femoral artery group. In
addition, higher troponin I and C-reactive protein and lower
albumin levels were also noted in the femoral artery group (
p
<
0.05). The survivors in the subclavian artery group had a shorter
mean ventilator-dependent duration (6.0
±
4.8 vs 6.4
±
3.5 days)
as well as ICU (8.9
±
5.8 vs 13.3
±
9.1 days) and hospital stay (18.8
±
9.8 vs 34.1
±
22.6 days) than those in the femoral artery group.
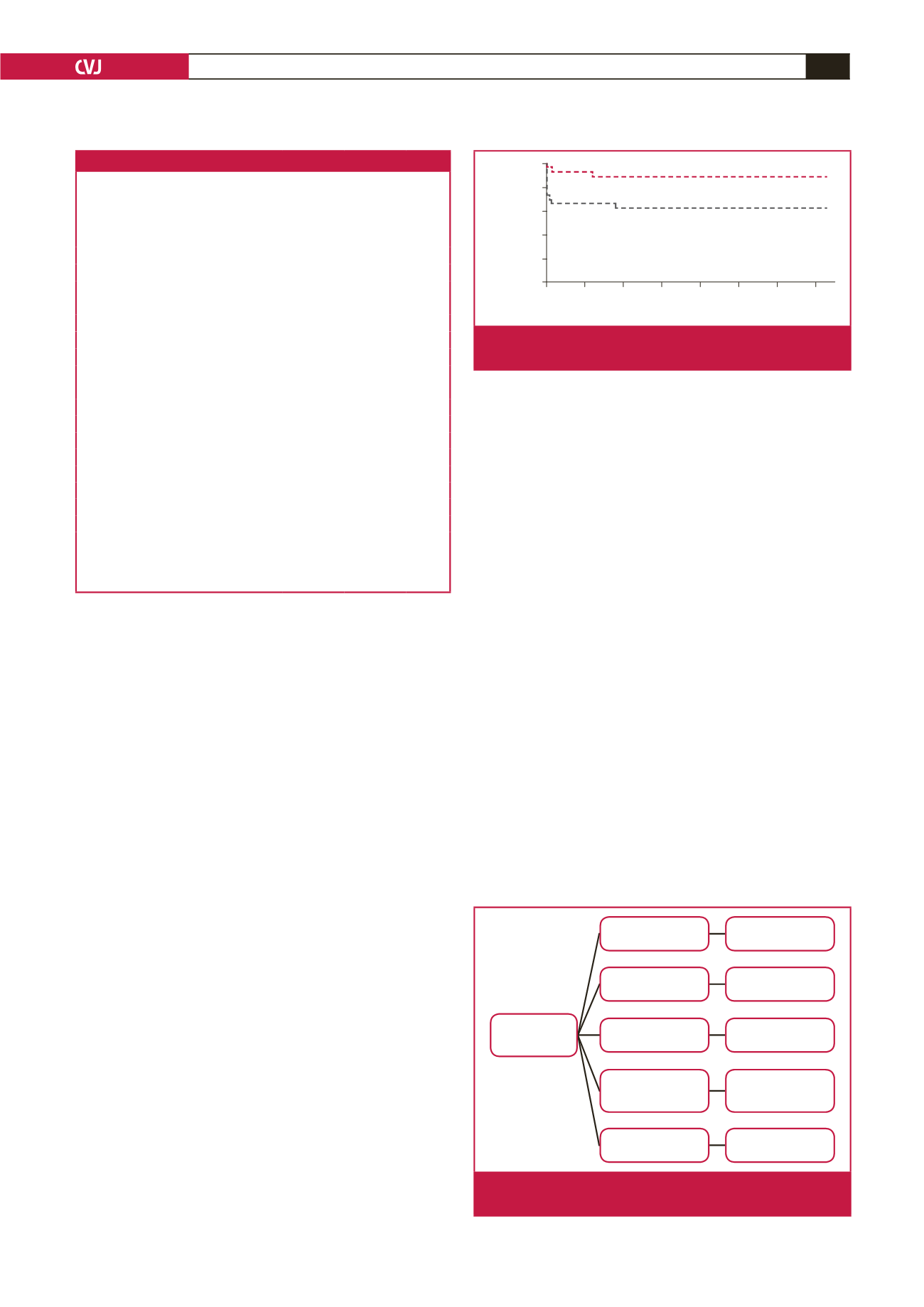
The compared Kaplan–Meier survival curve for the two
groups is shown in Fig. 1. All 40 survivors were followed up
for three years with annual CT angiography. Two patients died
within one year of surgery, one of sudden death and the other
of a cerebral vascular accident. Two more patients died within
the next two years, one of pneumonia with severe sepsis and the
other following recurrent dissection of the aortic root.
According to the outcomes of the annual CT angiography
(Fig. 2), three root re-dissections were found; two underwent
re-do Bentall’s operation and the other died of sudden death
without re-operation. Four arch dissections without branch
involvement were found and all four adopted conservative
treatment. Two arch aneurysms were found and one underwent
re-do arch reconstruction due to impending rupture. Three
dissecting aneurysms of the descending aorta were found and all
three underwent thoracic endovascular aortic repair (TEVAR).
The other 28 were diagnosed with type B dissection and adopted
conservative treatment. Overall survival was 75% at one year and
70% at three years.
Results of univariate and multivariate analysis are shown in
Table 3. Logistic regression analysis revealed independent risk
factors for hospital death as pre-operative respiratory failure,
peri-operative CPB
>
200 min, postoperative severe acidosis (pH
<
7.2), and troponin I
>
2.0 ng/ml.
Discussion
There is a trend towards cannulation of the axillary artery for
extracorporeal circulation in patients with AADA,
1-4
but the
debate is ongoing and several possible reasons could explain this
deficiency, including the following: (1) the urgency of AADA
does not allow for complicated surgical techniques but instead
requires a simple, rapid and safe approach to achieve rapid
extracorporeal circulation; (2) the different individual situations
demand an individual approach, and it is difficult to relate
outcome to the cannulation site; (3) the number of procedures
performed at each centre is rather small, especially in Asia, while
a multicentre approach is not practicable owing to the different
strategies practiced at different centres; and (4) most important
of all, the severity of the AADA hinges on the location of the
torn intima and the extent of the dissection, which also demands
different types of procedures. In this study, we enrolled only
cases involving ascending aorta reconstruction to avoid major
Table 2. Post-operative general data and short-term outcomes
Postoperative data
Total
Femoral
group
(
n
=
26)
Subclavian
group
(
n
=
25)
p
-value
pH
7.26
±
0.15 7.35
±
0.05 0.01
PaO
2
(mmHg)
115
±
92 136
±
75 0.37
HCO
3
-
(mEq/dl)
20.5
±
4.5 22.6
±
3.1 0.06
Amylase (U/l)
316
±
482 101
±
159 0.04
Lipase (U/l)
98
±
158 41
±
57 0.09
GOT (U/l)
391
±
1078 70
±
113 0.14
GPT (U/l)
286
±
890 33
±
29 0.16
Troponin I (ng/ml)
7.5
±
11.9 0.1
±
0.3 0.003
CRP (mg/dl)
10.9
±
8.0 5.4
±
3.5 0.003
Albumin (g/dl)
2.9
±
0.4 3.3
±
0.4 0.001
Short-term outcomes
Total number,
n
(%)
51
26 (100)
25 (100)
Transfusion
>
500 ml,
n
(%)
26 (51)
15 (57)
11 (44)
0.32
Resternotomy,
n
(%)
4 (8)
2 (7)
2 (8)
1.00
Mediastinitis,
n
(%)
2 (4)
2 (7)
0 (0)
0.01
Neurological dysfunction,
n
(%)
5 (9)
5 (19)
0 (0)
0.001
Pneumonia,
n
(%)
12 (23)
8 (27)
4 (16)
0.36
ARDS,
n
(%)
5 (9)
3 (11)
2 (8)
0.67
Acute renal failure,
n
(%)
22 (43)
15 (57)
7 (28)
0.03
Mortality,
n
(%)
11 (21)
9 (34)
2 (8)
0.04
The biochemical tests were recorded 24 hours after surgery. GOT, glutamate
oxaloacetate transaminase; GPT, glutamate pyruvate transaminase; CRP,
C-reactive protein; ARDS, acute respiratory distress syndrome.
0 50 100 150 200 250 300 350
Days
Cum survival
1.0
0.8
0.6
0.4
0.2
0.0
Subclavian canulation
Femoral canulation
+
+
Fig. 1.
Kaplan–Meier survival curve in relation to the two
groups.
40 survivors
3 root re-dissection
4 arch dissection
2 arch aneurysm
3 dissecting
aneurysm of
descending aortic
28 type B
dissection
2 re-do Bentall’s
procedure
Conservative
treatment
1 re-do arch
reconstruction
3 TEVAR
Conservative
treatment
Fig. 2.
Outcomes of the annual CT angiography and follow-up
intervention.

















