
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 3, May/June 2016
144
AFRICA
no intimal tear was discovered over the aortic root or the arch,
simple reconstruction of the ascending aorta was done and the
patient was enrolled in our data set. In total there were 21 cases
of DeBakey type I and 30 of DeBakey type II (Table 1). Of these
51 cases, seven patients underwent concomitant re-suspension of
the aortic valve due to mild aortic regurgitation, noted during
pre-operative echocardiography.
The patients were divided into two groups based on their
arterial cannulation site. We collected the data retrospectively
and focused on mortality rate and short- and mid-term results
between the two cannulation groups. Operative mortality was
defined as death within 30 days after surgery. Of the survivors, we
compared ventilator-dependent days, intensive care unit (ICU)
stay, and hospital stay between the two subgroups. The patients
were scheduled for follow-up CT angiography every three months
in the first year and then every year for the next two years.
Demographics and pre-operative characteristics of all 51
patients (38 men and 13 women) are summarised in Table 1. The
mean age of the patients was 59.0
±
14.0 years (median: 60.5;
range: 33–87). All surgeries were performed on an emergency
basis within 12 hours of the onset of symptoms. Forty-two
patients (82%) had hypertension, 13 (25%) had congestive heart
failure, and seven (13%) had diabetes. With regard to clinical
presentations (Table 1), 12 patients (23%) were in shock (systolic
blood pressure
<
90 mmHg), 14 (27%) had haemopericardium,
and 11 (21%) had respiratory failure with ventilator support.
Two patients developed cerebral ischaemia (4%), six developed
visceral ischaemia (12%), 11 developed renal ischaemia (21%),
and four developed lower limb ischaemia (8%).
Surgical technique
Before 2005, our cannulation strategy for repairing AADA tended
towards more use of femoral artery cannulation. After 2005, the
strategy switched to more use of subclavian artery cannulation
because of developing familiarity with this technique. We
routinely used 8- or 10-mm T-grafts for cannulation to avoid
compromise of perfusion distally, and then performed median
sternotomy and dual-stage venous cannulation over the right
atrium.
Once cardiopulmonary bypass (CPB) was initiated, profound
hypothermia was induced until the bladder or oesophageal
temperature was less than 18°C. At the same time, protective
adjuncts, such as barbiturates, steroids, ice packed around the
head, and steep Trendelenburg positioning, were employed for
cerebral protection. Aortic clamping was abandoned to avoid
injury to the fragile intima. Once the temperature was below
18°C, hypothermic circulatory arrest without retrograde cerebral
perfusion was used in the femoral cannulation group, while
antegrade selective cerebral perfusion with arterial flow of 8–10
ml/kg/min was used in the subclavian cannulation subgroup.
Aortotomy approximately 3 cm above the sinus of Valsalva
was performed, and the aortic root and arch were carefully
inspected to determine the optimal procedure for each case. If
arch reconstruction, Bentall’s procedure or David’s procedure
was required, these patients were excluded from the study. St
Thomas cardioplegic solution was directly infused via both
coronary ostia for myocardial protection. Distal anastomosis
with a Hemashield graft and sandwich procedure with Teflon
felt strips for reinforcement of the diseased aorta was performed
first, after which the perfusion was converted through the
ascending graft and was initiated to minimise systemic ischaemic
time. Proximal anastomosis was subsequently performed,
followed by rewarming, adequate de-airing, and weaning of the
extracorporeal circulation.
The intra-operative variables are summarised in Table 1.
Overall, the mean CPB time was 184.9
±
57.1 min, the mean
heart ischaemic time was 95.9
±
33.6 min, and the mean
circulatory arrest time was 32.2
±
5.4 min. In the femoral group,
without selective antegrade cerebral perfusion, the mean brain
ischaemic time was 33.8
±
5.1 min.
Statistical analysis
All statistical analyses were performed using SPSS software
version 12 (SPSS, Chicago, IL, USA). Categorical variables are
expressed as percentages and were evaluated with the
χ
2
test or
Fisher’s exact test. Continuous variables are expressed as mean
±
standard deviation and were evaluated using the Student’s
t
-test.
Stepwise logistic regression analysis was used to determine the
independent predictors of 30-day hospital mortality. Survival
was calculated by the Kaplan–Meier method.
Results
There were 11 (21%) deaths after surgery (Table 2), the causes of
which included cardiac failure in six, visceral ischaemia in three,
aortic re-dissection in one, and respiratory failure complicated by
adult respiratory distress syndrome (ARDS) in one. Five patients
(9%) had postoperative neurological complications, including
transient neurological dysfunctions in three and permanent
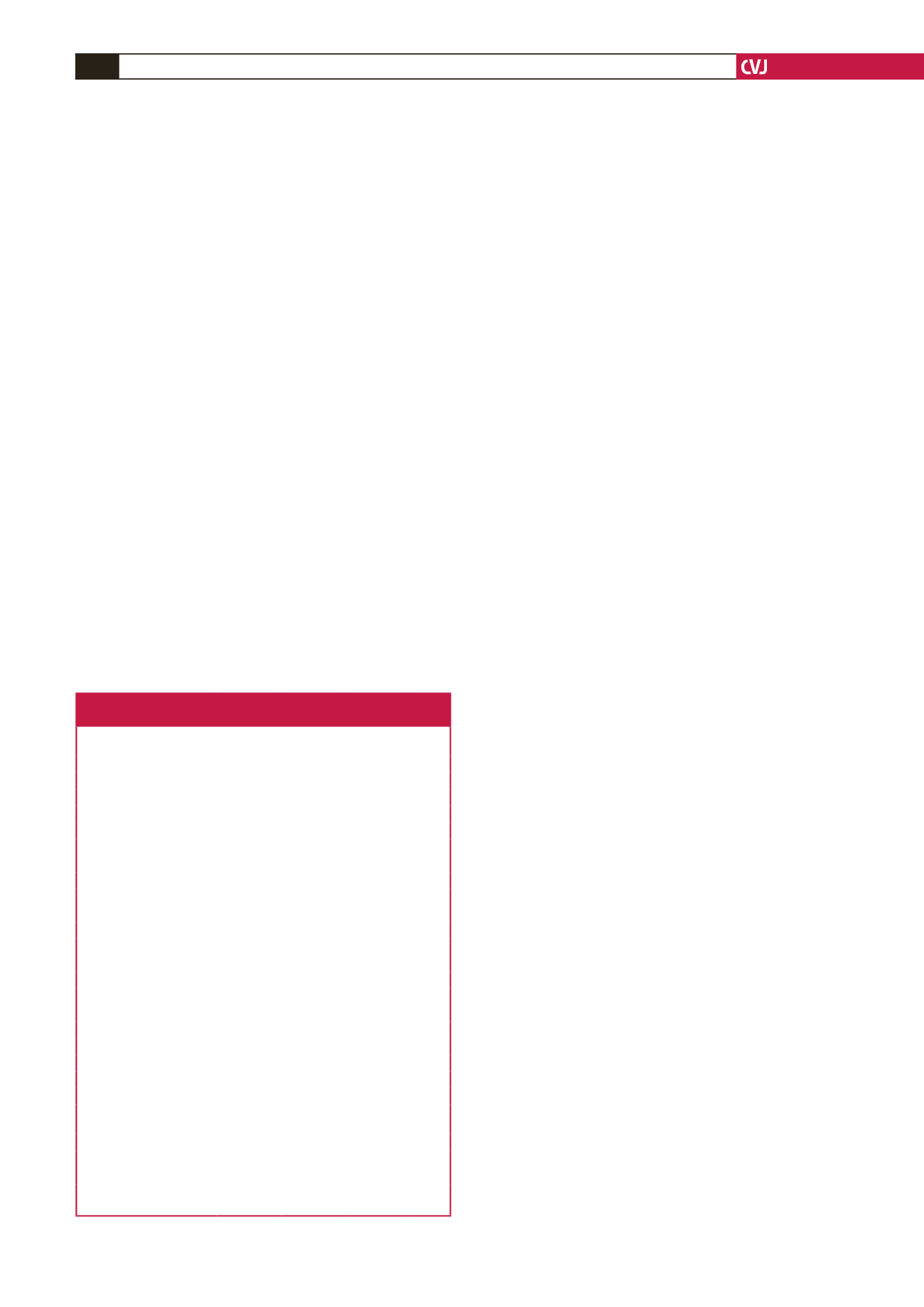
Table 1. Disease characteristics, clinical presentation
and intra-operative variables
Parameters
Total,
n
(%)
Femoral
group,
n
(%)
Subclavian
group,
n
(%)
p-
value
Total number
51
26 (100)
25 (100)
DeBaykey type I
21 (41)
12 (46)
9 (36)
DeBaykey type II
30 (59)
14 (54)
16 (64)
Age (mean
±
SD)
59.0
±
14.0 60.9
±
13.7 57.0
±
14.4 0.33
Gender (male)
38 (74)
20 (77)
18 (72)
0.687
Cerebral vascular accident
1 (2)
1 (4)
0 (0)
1.00
Coronary artery disease
8 (15)
4 (15)
4 (16)
1.00
Diabetes
7 (13)
4 (15)
3 (12)
1.00
Hypertension
42 (82)
23 (88)
19 (76)
0.24
PAOD
1 (2)
0 (0)
1 (4)
0.98
Congestive heart failure
13 (25)
8 (30)
5 (20)
0.37
COPD
6 (11)
2 (7)
4 (16)
0.62
Shock
12 (23)
7 (27)
5 (20)
0.56
Haemopericardium
14 (27)
10 (38)
4 (16)
0.138
Aortic regurgitation
7 (13)
6 (23)
1 (4)
0.11
Cerebral ischaemia
2 (4)
2 (7)
0 (0)
0.48
Respiratory failure
11 (21)
6 (23)
5 (20)
0.78
Visceral ischaemia
6 (12)
3 (11)
3 (12)
0.95
Renal ischaemia
11 (21)
6 (23)
5 (20)
0.78
Limb ischaemia
4 (8)
2 (7)
2 (8)
0.96
Operation time (h)
7.13
±
1.60 7.53
±
1.72 6.72
±
1.39 0.07
Cardiopulmonary bypass
time (min)
184.9
±
57.1 177.9
±
62.1 192.2
±
51.6 0.37
Heart ischaemic time (min)
95.9
±
33.6 97.0
±
34.5 94.8
±
33.3 0.81
Circulatory arrest time (min) 32.2
±
5.4 33.8
±
5.1 30.6
±
5.3 0.03
Brain ischaemic time (min)
–
33.8
±
5.1
0
0.00
PAOD, peripheral arterial occlusion disease, COPD, chronic obstructive pulmo-
nary disease.

















