
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 5, September/October 2016
AFRICA
313
In our study, systolic function of the left ventricle, wall
thickness, left ventricular diameters, volumes, and cardiac
index measurements were within normal limits. There were no
statistically significant differences between the Wilson’s disease
patients and the control group for left ventricular systolic
function, wall thickness, diameter, volume and cardiac index (
p
>
0.05). Our patients were relatively young and the mean age at
diagnosis was 9
±
2.24 years, so their time from diagnosis was
relatively short. Cardiac systolic function may deteriorate in the
long term or due to serious disease.
Tissue Doppler echocardiography, strain and strain rate
echocardiography are relatively novel echocardiographic
techniques and important tools to assess asymptomatic
patients.
11-14
Tissue Doppler imaging, which has recently allowed
a detailed examination of cardiac function, is widely used to
evaluate children with various conditions.
14-17
Our previous study
showed early diastolic dysfunction in patients with Wilson’s
disease using tissue Doppler echocardiography. Despite its
reliability, tissue Doppler echocardiography cannot show
regional deformation and regional deformation abnormalities.
Difficulties with angle dependency of tissue Doppler imaging,
the effects of preload, and the translational motion of the heart
were overcome by strain and strain rate echocardiography,
which were then adopted as new models in the assessment of
myocardial performance and local deformation properties.
13-15
Strain imaging, based on speckle tracking, in particular, enabled
assessment of myocardial motion and deformation irrespective
of angle and geometry, allowing an improved examination of the
myocardial mechanics.
Our hospital is a liver transplantation centre, therefore, we
aimed to assess a new group of children with Wilson’s disease
using 2D strain and strain rate echocardiography. Strain and
strain rate echocardiography are superior to tissue Doppler
echocardiography in the evaluation of regional myocardial
function because they are not affected by the translation and
stretching of neighbouring myocardial segments.
16
2D strain and
strain rate echocardiography also can assess different clinical
conditions, such as hypertension, obesity, post exercise, Marfan
syndrome, healthy children and infants.
15-18
To our knowledge, the literature presents no studies showing
early detection of subclinical cardiac dysfunction in children with
Wilson’s disease using 2D strain and strain rate echocardiography.
Our study showed that among the global strain and strain
rate parameters, Wilson’s disease patients had lower peak A
longitudinal velocity of the left basal point (VAbasL) and peak E
longitudinal velocity of the left basal (VEbasR) point than those
of the control group (
p
<
0.05). The patients also had statistically
significantly higher global peak A longitudinal/circumferential
strain rate (GSRa) (
p
<
0.05).
Longitudinal strain and strain rate from the four-chamber
view showed that end-systolic longitudinal strain [SLSC
(ES)] and positive peak transverse strain (STSR peak P) were
statistically significantly lower in the patient group (
p
<
0.05).
Radial strain and strain rate analysis showed that end-systolic
rotation [ROT (ES)] was statistically significantly lower in the
patient group (
p
<
0.05). Longitudinal strain and strain rate from
the two-chamber view showed that end-systolic longitudinal
strain [SLSC (ES)] and positive peak transverse strain (STSR
peak P) were statistically significantly lower in the patient group
(
p
<
0.05).
Segmental analysis also showed that rotational strain
measurement of the anterior segment of the patient group,
end-systolic longitudinal strain [STSR (ES)] of the basal lateral
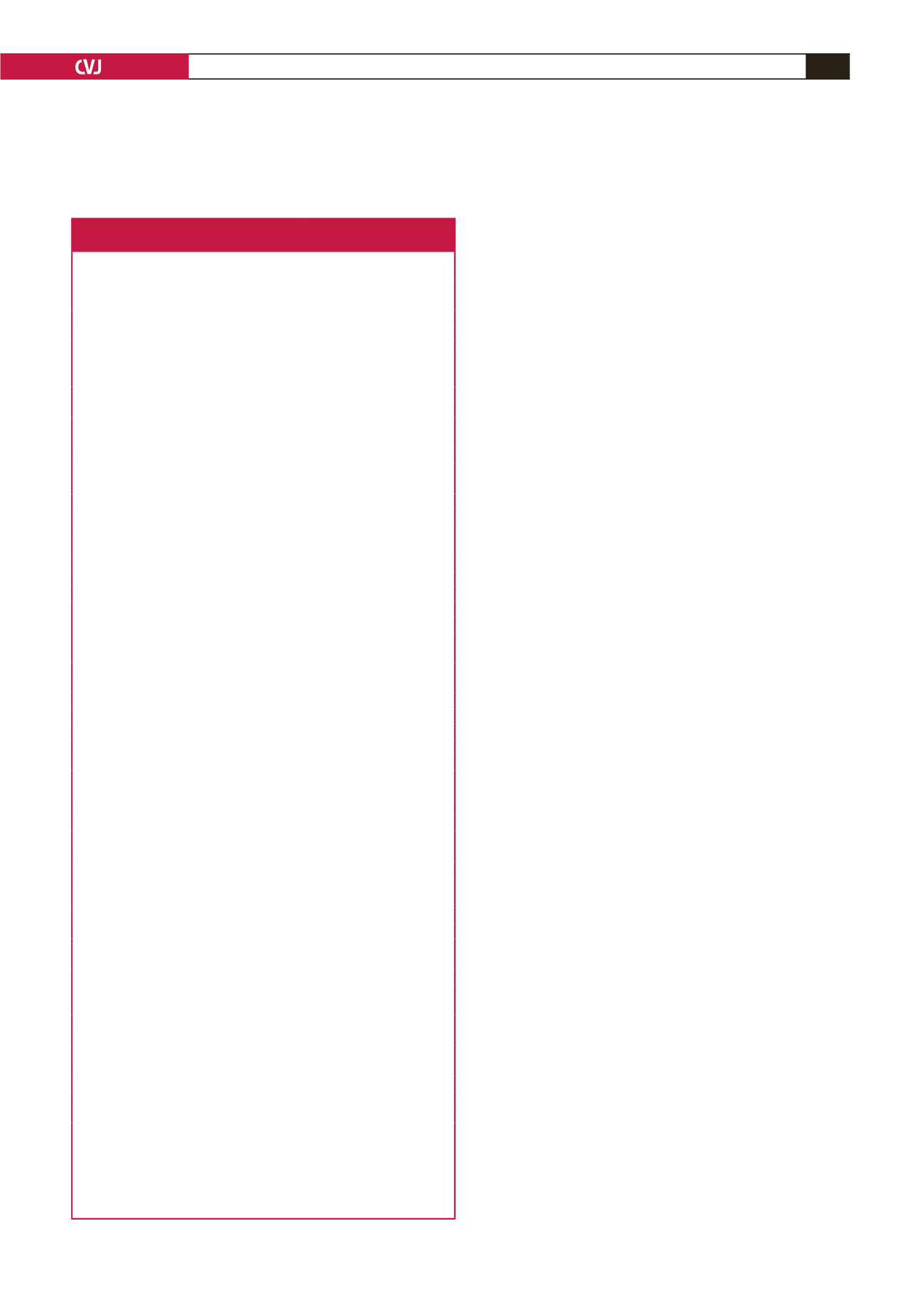
Table 8. Longitudinal and transverse strain and strain rate values
according to segment from the apical long-axis view
Strain according to
segment
Patients (
n
=
21)
(mean
±
SD)
Controls (
n
=
20)
(mean
±
SD)
p
-value
SLSCC peak G (%)
Basal anterior septal
–19.99
±
2.75
–18.63
±
5.80
0.24
Basal posterior
–16.60
±
11.17
–15.34
±
5.24
0.58
Mid-posterior
–18.27
±
3.83
–17.08
±
3.20
0.20
Apical posterior
–17.94
±
4.47
–17.73
±
4.48
0.86
Apical anterior septal
–15.33
±
5.55
–16.56
±
6.86
0.46
Mid-anterior septal
–18.01
±
2.58
–17.72
±
5.69
0.80
SLSC peak S (%)
Basal anterior septal
–19.68
±
3.06
–18.45
±
5.81
0.31
Basal posterior
–16.29
±
10.74
–15.06
±
5.42
0.59
Mid-posterior
–17.98
±
4.10
–17.018
±
3.14
0.32
Apical posterior
–17.39
±
4.56
–17.44
±
4.80
0.96
Apical anterior septal
–14.91
±
5.32
–16.21
±
6.88
0.43
Mid-anterior septal
–17.82
±
2.71
–17.64
±
5.65
0.87
SLSC peak P (%)
Basal anterior septal
0.25
±
0.81
0.125
±
0.28
0.42
Basal posterior
2.88
±
8.90
2.07
±
2.08
0.64
Mid-posterior
0.16
±
0.49
0.43
±
0.69
0.08
Apical posterior
0.15
±
0.29
0.17
±
0.42
0.84
Apical anterior septal
0.22
±
0.36
0.30
±
0.68
0.61
Mid-anterior septal
0.02
±
0.06
0.14
±
0.35
0.07
STSR peak P (%)
Basal anterior septal
21.30
±
22.17
29.87
±
24.35
0.16
Basal posterior
35.91
±
26.93
34.86
±
25.61
0.88
Mid-posterior
27.98
±
23.49
27.18
±
18.86
0.88
Apical posterior
21.76
±
18.45
21.56
±
14.17
0.96
Apical anterior septal
19.14
±
16.83
20.87
±
13.64
0.67
Mid-anterior septal
18.56
±
18.17
24.07
±
19.07
0.26
STSR peak G (%)
Basal anterior septal
–19.54
±
3.04
–18.38
±
5.85
0.39
Basal posterior
–16.04
±
11.32
–14.81
±
5.47
0.60
Mid-posterior
–17.89
±
4.14
–16.87
±
3.17
0.29
Apical posterior
–17.19
±
4.63
–17.30
±
4.75
0.92
Apical anterior septal
–14.66
±
5.51
–16.09
±
6.82
0.39
Mid-anterior septal
–17.68
±
2.84
–17.59
±
5.66
0.93
SLSC (ES) (%)
Basal anterior septal
14.59
±
24.85
24.53
±
25.34
0.13
Basal posterior
28.05
±
27.70
28.55
±
28.82
0.94
Mid-posterior
24.35
±
23.59
23.42
±
21.06
0.87
Apical posterior
20.06
±
19.09
20.12
±
14.95
0.99
Apical anterior septal
17.58
±
17.78
19.77
±
14.08
0.61
Mid-anterior septal
15.53
±
20.06
21.84
±
19.12
0.22
STSR (ES) (%)
Basal anterior septal
10.95
±
3.58
11.50
±
3.49
0.55
Basal posterior
13.75
±
3.59
11.37
±
2.26
0.004
Mid-posterior
8.81
±
2.56
7.20
±
1.59
0.0006
Apical posterior
3.23
±
1.26
2.27
±
1.216
0.005
Apical anterior septal
1.28
±
1.61
2.21
±
2.46
0.10
Mid-anterior septal
5.55
±
2.96
6.56
±
3.34
0.23
DLDC (ES) (mm)
Basal anterior septal
1.77
±
2.00
2.62
±
2.11
0.11
Basal posterior
4.91
±
2.08
3.57
±
1.57
0.008
Mid-posterior
3.97
±
1.59
2.95
±
1.37
0.012
Apical posterior
2.46
±
1.34
2.24
±
1.31
0.53
Apical anterior septal
1.56
±
1.37
2.17
±
1.55
0.12
Mid-anterior septal
1.55
±
1.50
2.54
±
1.81
0.027
SLSC peak G: the most negative peak longitudinal strain, SLSC peak S: negative
systolic peak longitudinal strain, SLSC peak P: positive systolic peak longitudinal
strain, SLSC (ES): end-systolic longitudinal strain, STSR peak P: positive peak
transverse strain, STSR peak G: the most negative peak transverse strain, STSR
(ES): end-systolic longitudinal strain, DLDC (ES): end-systolic longitudinal
displacement.

















