
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 1, January/February 2017
AFRICA
61
is mostly caused by hypertension and not by coronary artery
disease, as is seen in Western countries.
4
Patients with HF are heterogeneous in terms of risk of
cardiac death and re-admission for decompensated HF. Therefore
assessment of prognosis is a fundamental step in individual patient
management. Analysis of clinical variables has helped in identifying
the most significant predictors of mortality in the HF population.
5
Echocardiography has become the gold standard for the
evaluation of patients with HF because it is an inexpensive,
highly reproducible, widely available and relatively extensive
method for assessing left ventricular systolic and diastolic
function.
6
In fact, the recent HF guidelines of the European
Society of Cardiology state that ‘echocardiography is the method
of choice in patients with suspected HF for reasons of accuracy,
availability (including portability), safety, and cost’.
7
More than 20 echocardiographic parameters have been
proposed as predictors of outcome in HF patients in a number
of clinical studies.
8
However, the role of echocardiography in
the assessment and risk stratification of acute HF has been less
clear. Some small studies have found little correlation between
echocardiographic and haemodynamic variables in acute HF,
and little change in these variables from admission to follow
up.
9
In large registries and trials, echocardiographic parameters
were not found in many cases to be associated with outcomes.
10
Therefore, it is not clear which echocardiographic variables are
of importance in patients with acute HF.
5,11
THESUS-HF
3
provided a unique opportunity to study the
echocardiographic predictors of outcome in patients admitted with
acute HF in this part of the world. To our knowledge, no similar
study has been previously published in Africans with acute HF.
Methods
THESUS-HF was a prospective, multicentre, international
observational survey of acute HF in 12 cardiology centres from
nine countries in sub-SaharanAfrica.
3
All participating centres had
a physician trained in clinical cardiology and echocardiography.
Patients who were older than 12 years, were admitted with
dyspnoea as the main complaint, and were diagnosed with
acute HF based on symptoms and signs that were confirmed
by echocardiography (
de novo
or decompensation of previously
diagnosed HF) were enrolled consecutively. Patients excluded
were those with acute coronary syndromes, severe known renal
failure (patients undergoing dialysis or with a creatinine level of
>
4 mg/dl), nephrotic syndrome, hepatic failure or other cause of
hypoalbuminaemia.
Written informed consent was obtained from each subject
who was enrolled into the study. Ethical approval was obtained
from the ethics review boards of the participating institutions,
and the study conformed to the principles outlined in the
Declaration of Helsinki.
Details of data collection have been previously described.
3
In
brief, we collected demographic data, detailed medical history,
vital signs (blood pressure, heart rate, respiratory rate and
temperature) and signs and symptoms of heart failure (oxygen
saturation, intensity of oedema and rales, body weight and levels
of orthopnoea). Assessments were done at admission and on
days 1, 2 and 7 (or at discharge if earlier).
Electrocardiograms were done and read using standard
reference ranges. A detailed echocardiographic assessment was
performed (see below). The probable primary cause of HF was
provided by the investigators, and was based on the European
Society of Cardiology guidelines,
7
as recently applied in the
chronic HF cohort of the Heart of Soweto Study.
12
Information
on re-admissions and death, with respective reasons and cause,
was collected throughout the six-month follow up. Outcomes of
interest were re-admission or death within 60 days, and death up
to 180 days.
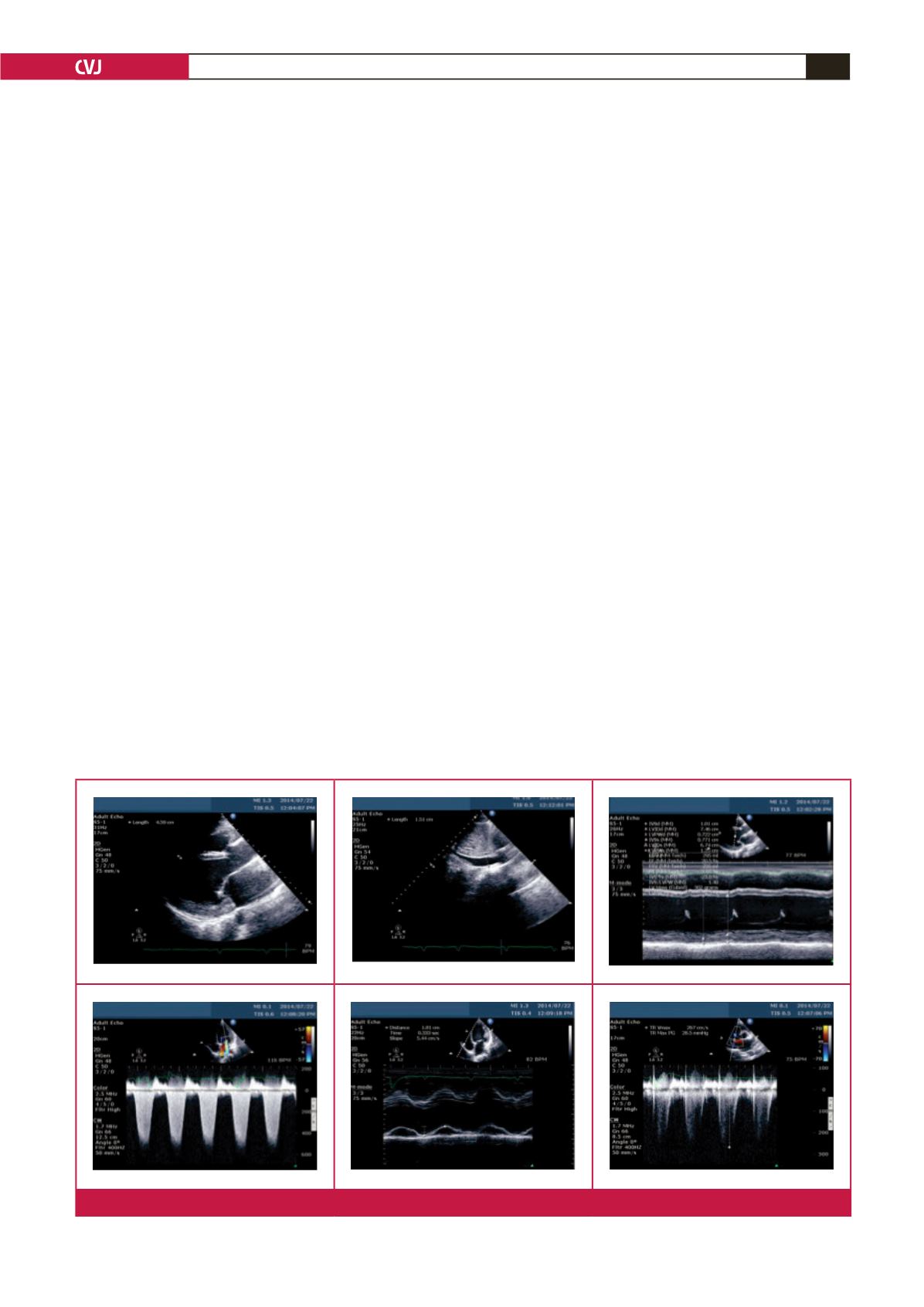
Fig. 1.
Echocardiography images depicting method of echo assessment in the study.

















