
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 2, March/April 2017
AFRICA
129
patient’s risk of CHD, therefore necessitating an integrated,
multi-faceted therapeutic approach.
In this section, the pathogenetic pathways activated by
moderate exercise are described, but the effects of these pathways
have not been quantified. The next interrogation was therefore
whether biomarkers could quantify the CHD effect of moderate
exercise. This was accomplished by using connection graphs,
which link the relative effect of a health or pathogenic factor to
the individual biomarkers through the pathways that are shown
in Fig. 1.
Biomarkers of coronary heart disease
The integrated model that was developed is a high-level
conceptual model, from which the interconnectedness of CHD is
immediately apparent (Fig. 1). Themodel is however complicated.
Biomarkers can be used as indicators of an underlying disorder
and the measurement of specific biomarkers enables prediction
of the RR for CHD associated with the biomarker.
29-31
The
relevant biomarkers and their association with CHD risk per one
standard deviation increase in said biomarker are given in Table
2. This can allow for the quantification of the effects of moderate
exercise on the pathogenesis of CHD.
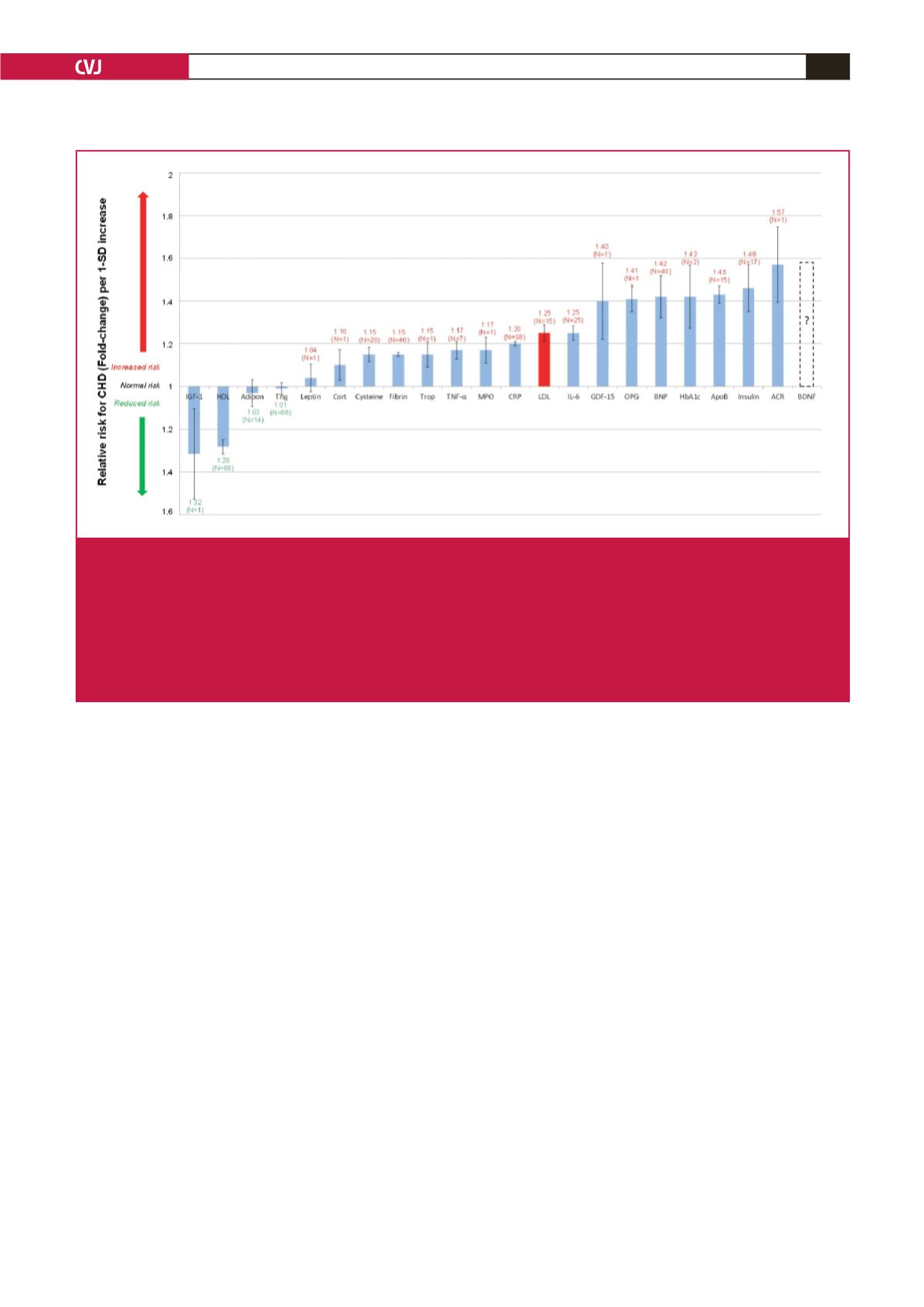
To simplify the integrated model, serological biomarkers
(which can easily be measured) are used to link the effect of
exercise to the corresponding RR of CHD. Fig. 2 presents a
comparison of the RR associated with an array of serological
biomarkers per one standard deviation increase in the biomarker.
7
Effects of moderate exercise
Using the integrated model in Fig. 1, it is possible to account
for the impact that moderate exercise would have on the
serological biomarkers of CHD. This enables a simplification of
the integrated model into a connection graph, which shows all
the connections between moderate exercise and the measurable
serological biomarkers.
The connection graph presented in Fig. 3 does not neglect
any of the underlying complexity of CHD. To more clearly
determine the effect of exercise on different biomarkers in Fig.
3, the biomarkers previously shown in Fig. 2 were divided into
eight classes, namely vascular function and neurohormonal
activity, renal function, necrosis, coagulation, oxidative stress,
lipids, and metabolic and inflammatory markers.
The pathogenetic pathways (from Fig. 1) are superimposed
on the connecting lines in Fig. 3. Increasing line thickness
indicates a connection with possible greater pathogenetic effect
(as quantified by biomarker relative-risk prediction of CHD).
For example, the risk of CHD is relatively low when considering
leptin, therefore the connection line between exercise and leptin
is thinner than for others (e.g. Apo B).
It is intriguing to see that moderate exercise has a connection to
all the serological biomarkers. This further highlights the inverse
correlation between CHD risk and moderate exercise. From the
connection graph in Fig. 3, it can be noted that the potential risk
reduction effect of moderate exercise may be greatly influenced
by changes in inflammatory, metabolic and lipid markers, which
provide a considerable increased risk for CHD.
2-4
Fig. 2.
Normalised relative risks (fold-change) of salient current biomarkers or of potential serological biomarkers for CHD. (From:
M Mathews, L Liebenberg, E Mathews. How do high glycemic load diets influence coronary heart disease?
Nutr Metab
2015; 12(1): 6.
7
)
Increased IGF-1 and HDL levels are associated with a moderately decreased CHD risk. (IGF-1 and HDL
levels are significantly inversely correlated to relative risk for CHD.)
N
indicates number of trials; I, 95% confidence inter-
val; ACR, albumin-to-creatinine ratio; Adipo, adiponectin; ApoB, apolipoprotein-B; BDNF, brain-derived neurotrophic factor;
BNP, B-type natriuretic peptide; Cort, cortisol; CRP, C-reactive protein; cysteine, homocysteine; fibrin, fibrinogen; GDF-15,
growth-differentiation factor-15; HbA
1c
, glycosylated haemoglobin A
1c
; HDL, high-density lipoprotein; IGF-1, insulin-like growth
factor-1; IL-6, interleukin-6; LDL, low-density lipoprotein; MPO, myeloperoxidase; OPG, osteoprotegerin; TNF-
α
, tumour
necrosis factor-
α
; Trigl, triglycerides; Trop, troponins.

















