
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 2, March/April 2018
90
AFRICA
presentations in this group included claudication (31%), rest pain
(13.8%) as well as neurovascular symptoms (6.9%).
Surgical interventions
Ninety-five procedures were performed in 64 patients. Of these,
89 were open procedures with six cases managed by means of an
exclusively endovascular approach. A distinction should be made
between minor procedures (10 in total; wound debridements,
evacuation of haematomas, closure of fasciotomy wounds and
excision/ligation of bypass grafts), attempts at revascularisation
(77 in total; see Table 2) and ablative procedures (18 in total; see
Table 3).
Surgical outcome was reported by quantifying the mortality,
morbidity and amputation rates, and functional outcome at
certain time intervals post-initial procedure. Unfortunately,
follow-up appointments were poorly attended, restricting the
interpretation of long-term data (Table 3).
In the first 30 days, 18 amputations were performed in 64
patients. Ten amputations were performed primarily (at initial
surgical procedure) in patients presenting with irreversible tissue
necrosis. Eight secondary amputations (four major, four minor)
were performed within 30 days following an initial attempt at
revascularisation. A total of six patients (9.4%) required a major
amputation at 30 days, of whom three presented with acute ULI.
At six month’s follow up, five patients presented with bypass
graft occlusion (resulting in one above-elbow amputation)
and one with re-occlusion of native vessels post-embolectomy.
Functionally, four patients presented with contractures, one with
motor weakness (affecting activities of daily living) and two with
claudication. Twenty-three patients were assessed as having a
fully functional ipsilateral upper limb.
After six months, one patient developed bypass graft occlusion
as part of an agonal event. Thirteen patients reported normal
function, two presented with contractures, one with persistent
motor weakness and one with claudication symptoms.
Five patients died within 30 days of admission, resulting in a
30-day all-cause mortality rate of 7.8%. No further mortalities
or systemic complications were noted at the six-month follow
up. One patient died of lung carcinoma two years after initial
presentation with ULI.
Discussion
We report on the first institutional experience with surgical
management of ULI from the African continent, in an attempt
to identify ethnic, demographic and geographic confounders.
However, several research limitations resulted in the generation
of multiple, tentative assumptions to direct future research,
rather than robust scientific conclusions.
Firstly, by attempting to discuss distinctly different
aetiopathological processes in unison, important individual
characteristics may be obscured. Adherence to follow up was
poor, limiting the interpretational value of long-term data. With
this in mind, a few relevant findings will be discussed.
The true incidence of ULI in South Africa remains
speculative. A major limiting factor is the paucity of data
on non-surgical management of ULI. In the current series,
subjects were retrospectively selected from a surgical database
without capturing those managed non-surgically. The single-
centre nature of this series does not allow for any firm conclusion
regarding the regional and race-specific incidence of ULI as the
number and ethnicity of patients seeking medical attention from
private healthcare facilities are currently unknown.
Despite the above-mentioned limitations, a clear escalating
trend was observed, with 56% of surgically managed patients
referred within the last four years of the study period. An increase
in the absolute number of referrals is the most conceivable
explanation for the observed trend. A less likely explanation
may be that a more aggressive surgical approach was followed
during the last four years of the study. Anecdotally though, the
indications for surgical intervention have remained unchanged.
The largest surgical series investigating patients undergoing
revascularisation procedures for ULI was published by Deguara
et al
.
1
in 2005. A total of 172 patients were included over a
20-year period, with 53 cases related to upper-extremity trauma
(excluded in the current series). Comparison of data between
the two series makes for interesting discussion, especially when
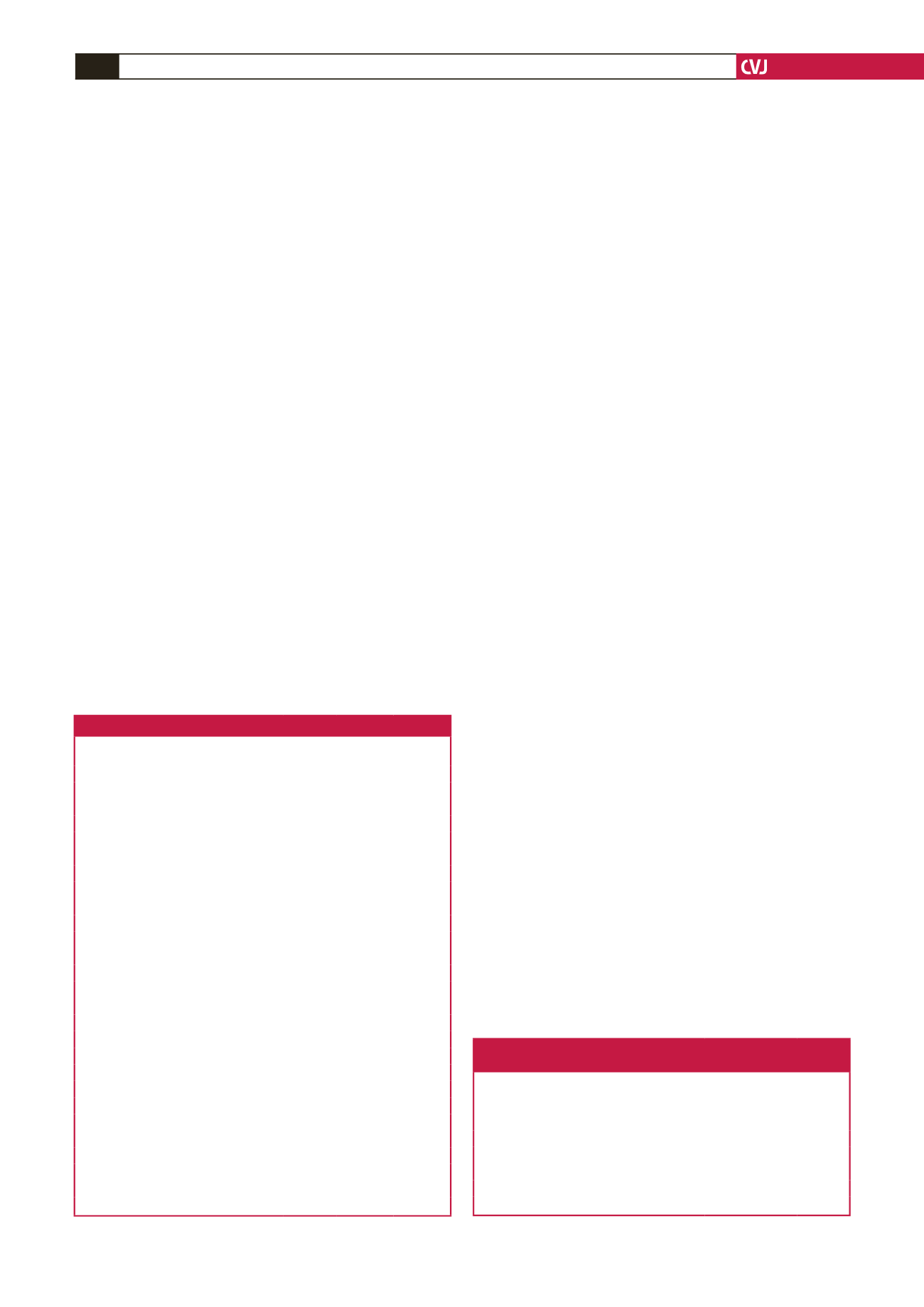
Table 3. Summary of 30-day, six-month and long-term outcome
Outcome measure
30-day
n
(%)
6-month
n
(%)
Long-term
n
(%)
Adherence to follow up
53 (83.0) 30 (50.8) 17 (28.8)
Mortality
5 (7.8)
–
1
Acute coronary syndrome
2
Acute kidney injury
2
Acute respiratory failure
1
Morbidity
Systemic complications
8 (12.5)
–
–
Acute kidney injury
3
Acute respiratory insufficiency
3
Acute coronary syndrome
1
Cerebrovascular incident
1
Procedural complications
18 (23.4)
7
1
Surgical site haematoma
6
Superficial surgical site infection
4
Bypass graft occlusion
3
5
1
Pseudo-aneurysm post-angiogram
2
Delayed fasciotomy
1
Neuropraxia
1
1
Re-thrombosis of native vessels
1
1
Amputation rate
Primary amputation (2 major, 8 minor)
10 (15.6)
Secondary amputation (4 major, 4 minor) 8 (12.5)
1
Functional outcome
Normal
23
13
Contracture
4
2
Claudication symptoms
2
1
Motor weakness
1
1
Table 4. Demographic and outcome comparisons of thrombo-embolic
and atherosclerotic occlusive disease
Number
Mean age
(years)
M:F
ratio
30-day
mortality
rate (%)
Amputa-
tion rate
(%)
Current series
Thrombo-embolic
30
55
1:2.3
16.7
13.3
Atherosclerotic occlusive 12
57
1:1.4
0
8.3
Deguara
et al
.
1
Thrombo-embolic
61
72
1:1.1
18.2
0
Atherosclerotic occlusive 29
63
1:1.9
6.9
0

















