
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 2, March/April 2018
96
AFRICA
liver disease.
3
Fatty liver disease and the metabolic syndrome
share many pathophysiological mechanisms and co-morbidities,
such as dyslipidaemia, type 2 diabetes mellitus, insulin resistance
and obesity.
As demonstrated in our study, patients with fatty liver disease
had more metabolic co-morbidities than those without fatty liver
disease. The metabolic syndrome promotes the progression of
atherosclerosis and increases the risk of cardiovascular disease.
23
Moreover, fatty liver disease has been found to be associated with
increased mortality rates due to cardiovascular disease and was
an independent risk factor for atherosclerosis.
24,25
The association
of fatty liver disease with the development of cardiovascular
disease indicates the importance of early detection and close
follow up of atherosclerosis in patients with fatty liver disease.
The goal of clinical medicine is to prevent as well as cure
disease. However, guidelines do not exist regarding which
method of screening should be performed in patients with
fatty liver disease and how often they should be evaluated to
prevent complications caused by atherosclerosis. Prior studies
have shown that the measurement of CIMT using carotid
ultrasound and of CACS using cardiac CT can detect subclinical
atherosclerosis in fatty liver disease patients.
9,26
Increased CIMT in the carotid artery reflects the onset of early
atherosclerotic change in the arterial wall. It is known that CIMT
measurement by carotid ultrasound in asymptomatic individuals
can independently predict future cardiovascular events.
27,28
Importantly, by showing a significant increase in CIMT values in
patients with fatty liver disease compared to those with a normal
liver, our study demonstrated that the development of subclinical
atherosclerosis had already been initiated in patients under 50
years of age with fatty liver disease. In addition, it revealed that
CIMT evaluation can effectively detect subclinical atherosclerosis
in patients with a CACS of zero or below 100. These findings
have important implications for screening and prevention of
cardiovascular disease in asymptomatic young patients.
An elevated CACS is also an independent risk factor
for coronary artery disease.
22
Moreover, as coronary artery
calcification is associated with a higher incidence of major and
minor cardiovascular events, CACS estimation may serve as
an important tool in cardiovascular risk assessment. Because
arterial calcification represents end-stage changes in vascular
atherosclerosis,
29
the absence of calcifications does not mean that
the artery is free of atherosclerosis or non-calcified plaque. Our
study also suggests that there was no significant difference in the
CACS or in the presence of carotid plaques between patients
with fatty liver disease and those with normal livers, despite a
difference in CIMT values. Prior studies have also demonstrated
that coronary artery calcification was more strongly correlated
with carotid plaque burden than with CIMT values in patients
with asymptomatic subclinical atherosclerosis.
30,31
In earlier studies, the CACS has been shown to be the best
predictor of total cardiovascular disease, while the CIMT or
presence of carotid plaque have been found to be slightly better
than the CACS in predicting cerebrovascular events.
32-34
Both
cardiovascular and cerebrovascular events can be especially
catastrophic for young patients with underlyingmetabolic disease.
Therefore, a sensitive method for early detection of subclinical
atherosclerosis is needed for patients with fatty liver disease in
order to predict the likelihood of vascular complications and to
intervene with preventative therapies.
The main limitation of this study is that inclusion required
that patients had all examinations performed, including carotid
and abdominal ultrasound and calcium score CT, therefore our
results may not be generalisable to other subjects with the same
clinical characteristics. Another limitation of this study is its cross-
sectional design. A long-term, causal study is needed to assess the
impact of atherosclerosis screening on patient outcomes.
Conclusion
CIMT was a better marker of underlying subclinical
atherosclerotic risk among patients with fatty liver disease
than CACS. The measurement of CIMT was especially useful
in evaluating the risk of subclinical atherosclerosis in young
patients less than 50 years of age. Young patients with fatty liver
disease should undergo screening CIMT to detect atherosclerosis
so that their risk factors can be modified.
References
1.
Neuschwander-Tetri BA. Nonalcoholic steatohepatitis and the meta-
bolic syndrome.
Am J Med Sci
2005;
330
(6): 326–335.
2.
Targher G, Arcaro G. Non-alcoholic fatty liver disease and increased
risk of cardiovascular disease.
Atherosclerosis
2007;
191
(2): 235–240.
3.
Ozturk K, Uygun A, Guler AK, Demirci H, Ozdemir C, Cakir M
, et al.
Nonalcoholic fatty liver disease is an independent risk factor for athero-
sclerosis in young adult men.
Atherosclerosis
2015;
240
(2): 380–386.
4.
Maurantonio M, Ballestri S, Odoardi MR, Lonardo A, Loria P.
Treatment of atherogenic liver based on the pathogenesis of nonalco-
holic fatty liver disease: a novel approach to reduce cardiovascular risk?
Arch Med Res
2011;
42
(5): 337–353.
5.
Yki-Jarvinen H, Westerbacka J. The fatty liver and insulin resistance.
Curr Mol Med
2005;
5
(3): 287–295.
6.
Yesilova Z, Yaman H, Oktenli C, Ozcan A, Uygun A, Cakir E
, et al.
Systemic markers of lipid peroxidation and antioxidants in patients
with nonalcoholic Fatty liver disease.
Am J Gastroenterol
2005;
100
(4):
850–855.
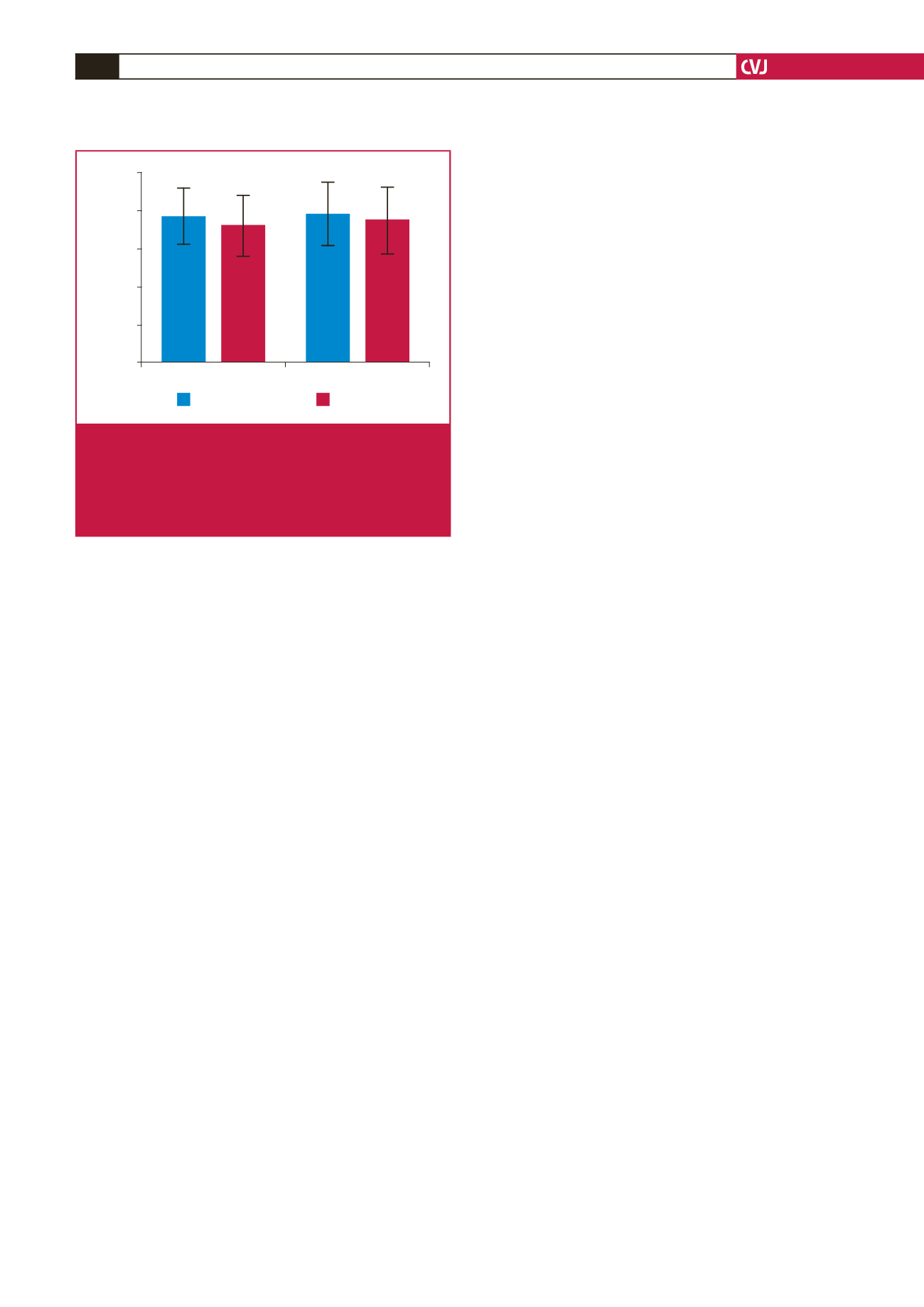
CACS 0
CACS <100
Carotid IMT (mm)
1.0
0.8
0.6
0.4
0.2
0.0
p = 0.002
p = 0.013
Fatty liver
Normal liver
Fig 1.
CIMT values according to the presence of fatty liver
disease in patients with a CACS of zero and less than
100. The mean CIMT value was significantly higher
among patients with fatty liver disease compared to those
with normal livers in both groups. CACS: coronary artery
calcium score; CIMT: carotid intima–media thickness.

















