
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 3, May/June 2018
AFRICA
e3
after a total of 18 days on Levitronix
®
haemodynamic support.
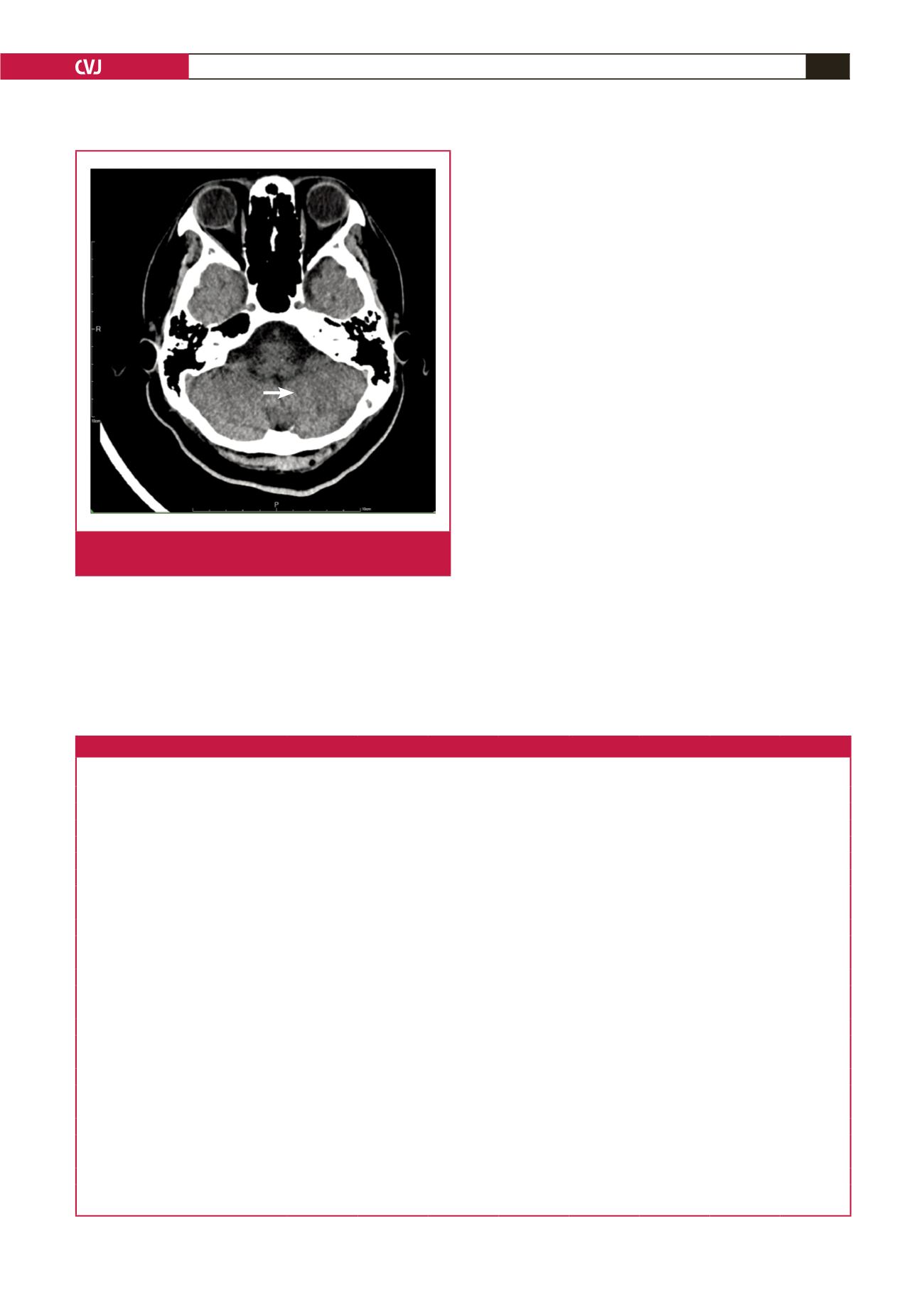
One week later, a tracheostomy was performed, and the patient
was weaned from the ventilator a week later. The follow-up CT
showed chronic encephalomalacia of the left cerebellum (Fig. 3).
The patient was discharged home 10 days later, after a total
hospital stay of 42 days. During out-patient follow up, no signs
of heart failure or device-related complications were noted.
Discussion
Before the use of VADs became popular, ECMO played an
important role in the haemodynamic support for decompensation
in cases of acute heart failure at our centre.
1,2
VADs provide
substantially longer durability and considerably fewer
complications than ECMO.
3-5
According to the 2016 guidelines
recommended by the International Society for Heart and Lung
Transplantation, clinically severe symptomatic cerebrovascular
disease may be considered a contraindication to transplantation.
6
Our policy was to use VADs as a bridge, either to recovery
or transplantation if the patient was able to recover from left
cerebellar infarction with right hemiplegia.
After starting VAD, high-dose inotropic support could be
tapered immediately (Table 1) to prevent vasoconstriction in
the vital visceral organs. During the period with VAD support,
both troponin-I levels and liver function progressively returned
to normal ranges. In time, cardiac function improved and the
VAD was successfully removed. Although renal function did not
recover promptly and haemodialysis was necessary during the
VAD period, the renal function did recover completely, albeit
two weeks later after VAD removal. This means that timely VAD
support could provide immediate circulatory support, enabling
cessation of high-dose inotrope administration, which would
cause vasoconstriction in the visceral organs, sequential ischaemia
of the visceral organs, and consequent multiple organ failure.
Currently, VADs can be categorised into two major
types: pulsatile-flow and continuous-flow VADs. We chose
the Levitronix
®
VAD for the following reasons. First, recent
studies showed better outcomes with continuous-flow VADs
than with pulsatile-flow ones. In addition, complications
associated with continuous-flow VADs, especially bleeding and
thromboembolism, are lower.
7,8
Table 1. Clinical time course
Before VAD POD1
POD2
POD3
POD6
POD9
POD12
POD15
POD18
VAD removal
Cardiac enzyme
BNP (pg/ml)
350
518
553
2219
1974
584
590
405
363
CK (U/l)
1743
2609
3098
3245
800
219
63
53
45
CKMB (U/l)
136.6
67.8
–
–
–
–
–
–
–
Troponin-I (ng/ml)
90.06
94.02
60.70
33.65
6.31
0.68
0.22
0.11
0.05
Renal function
BUN (mg/dl)
33
33
41
49
108
52
70
114
121
Creatinine (mg/dl)
3.4
3.6
4.6
4.7
7.7
5.3
3.8
3.6
3.1
Daily urine amount (ml)
0
128
250
545
1540
1120
1160
2550
2240
Liver function
GOT (U/l)
214
722
1191
795
133
94
47
52
40
GPT (U/l)
81
416
633
706
372
200
66
60
64
Total bilirubin (mg/dl)
4.0
2.7
3.6
3.2
2.5
1.4
1.8
2.5
2.0
Inotropic agent
Dopamine (mcg/kg/min)
15.0
5.1
5.1
3.0
1.8
2.9
4.7
4.4
7.6
Dobutamine (mcg/kg/min)
15.0
5.1
5.1
3.0
1.8
2.9
2.9
3.1
7.6
Epinephrine (mcg/min)
1.0
–
–
–
–
–
–
–
–
Norepinephrine (mcg/min)
32
3.7
–
–
2.0
1.6
1.2
–
–
VAD flow
Right (l/min)
2.7
3.5
3.2
3.0
3.0
2.8
1.6
Left (l/min)
4.5
5.0
5.0
5.0
5.0
4.8
2.6
VAD revolutions per minute
Right (/min)
3000
3000
2900
2900
2900
2700
1700
Left (/min)
4100
4000
3700
3700
3700
3500
2000
POD = post-operative day; VAD = left ventricular assist device; BUN = blood urea nitrogen; CK = creatinine kinase; CKMB = creatinine kinase MB coenzyme; GOT
= glutamic-oxaloacetic transaminase; GPT = glutamic-pyruvic transaminase.
Fig. 3.
The initial hypodense lesion progressed to chronic
encephalomalacia of the left cerebellum (white arrow).

















