
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 4, July/August 2018
248
AFRICA
closed with coils and with Amplatzer™ devices. Overall, the
PDAs where Amplatzer™ devices were used were bigger, with
larger shunts and higher pulmonary:systemic pressure ratios.
In about a third of patients, the fluoroscopy time for the
procedure had not been recorded. The median fluoroscopy time
for those with these data was 23.1 minutes, being similar with
coils and Amplazer placement. The shortest procedure took 8.3
minutes and the longest two hours 27 minutes.
Altogether, 150 transcatheter procedures were performed on
the 139 patients. More than 80% of patients required only
one procedure to effect closure (114), 16% required further
intervention (22) and no data on outcomes were available for 2%
of cases (three).
Twelve of the 22 patients who required further intervention
had a second catheterisation, eight of which were successful and
the other four had a residual PDA that was haemodynamically
insignificant and it was decided to observe them. A total of eight
patients required surgical closure (six with coils and two with
Amplazer devices). Two of the 22 were lost to follow up and no
further data were available.
Of the cases where complete PDA closure was documented on
echocardiography (117), closure had occurred within one week in
over 90% of the Amplatzer™ device cases, but in only half of the
procedures using coils (
p
<
0.001; Fig. 1). Overall, of the whole
cohort, no patients had a significant residual PDA in the long run.
A total of 101 COOK
®
coils were placed in 92 patients who
underwent transcatheter PDA closure with a coil (Fig. 2). In the
majority of patients, a single coil was used (74), however in larger
PDAs (before the Amplatzer™ devices were available) more than
one coil was occasionally required. In the 18 patients who required
more than one coil at their initial procedure, 13 had two coils, four
had three and one had four coils.
Overall, in 78% of patients with a known outcome, the PDA
was successfully closed with one or more coils (66/85). Surgical
closure was required in six patients where a coil was initially
attempted. Five patients had a small residual PDA that did
not require surgical closure, one PDA was noted to have closed
spontaneously at follow up, and seven patients were lost to follow
up.
Table 2. Characteristics of patent ductus arteriosus and haemodynamic
measurements in patients, by closure device
Variable
Total patients
(
n
=
139)
Coils
(
n
=
101)
Amplatzer™
devices
(
n
=
49)
p
-value
PDA size
Narrowest point,
mean (SD)
3.2 (1.6)
2.6 (1.1)
4.0 (1.9)
<
0.001
Size, % (
n/N
)
0.005
<
2.5 mm
37.5 (42/112)
47.8 (33/69)
21.7 (10/46)
≥ 2.5 mm
62.5 (70/112)
52.2 (36/69)
78.3 (36/46)
PDA shape
A, % (
n/N
)
72.8 (91/125)
74.1 (63/85)
72.9 (35/48)
0.82
B, % (
n/N
)
1.6 (2/125)
2.4 (2/85)
2.1 (1/48)
C, % (
n/N
)
5.6 (7/125)
3.5 (3/85)
8.3 (4/48)
D, % (
n/N
)
2.4 (3/125)
2.4 (2/85)
2.1 (1/48)
E, % (
n/N
)
17.6 (22/125)
17.7 (15/85)
14.6 (7/48)
Chest X-ray
Cardiomegaly,
% (
n/N
)
85.4 (111/130) 80.2 (73/91)
93.6 (44/47)
0.04
Plethora, % (
n/N
)
66.2 (86/130)
56.0 (51/91)
83.0 (39/47)
0.002
Haemodynamics
Pulse pressure,
mean mmHg (SD)
46.6 (9.6)
44.9 (10)
48.8 (8.5)
0.03
LA:AO*, mean (SD)
1.6 (0.4)
1.6 (0.4)
1.7 (0.4)
0.5
Shunt, (Qp:Qs)
mean (SD)
2.0 (1.2)
1.8 (0.8)
2.5 (1.6)
<
0.001
Pulmonary resistance
(Woods units), mean
(SD)
2.1 (1.8)
2 (1.9)
2.2 (1.6)
0.5
Pulmonary pressure:
systemic pressure
ratio mean (SD)
0.39 (0.2)
0.4 (0.1)
0.5 (0.2)
<
0.001
Fluoroscopy time
Median minutes,
(IQR)
23.1
(15.3–31.6)
21.3
(14.7–29.8)
23.5
(16.8–32.4)
0.55
N
varied due to missing data. The total sum of coils and Amplatzer devices
exceeded the number of patients as more than one device was used in some
patients. SD: standard deviation; IQR: interquartile range.
Amplatzer (
n
=
42)
Coil (
n
=
75)
p
<
0.001
<1 week 1 week –
6 months
6 months –
1 year
1–2 years > 2 years
Percentage closed
100
80
60
40
20
0
92.9
52.0
20.0
18.7
4.8
2.4
6.7
0.0
2.7 0.0
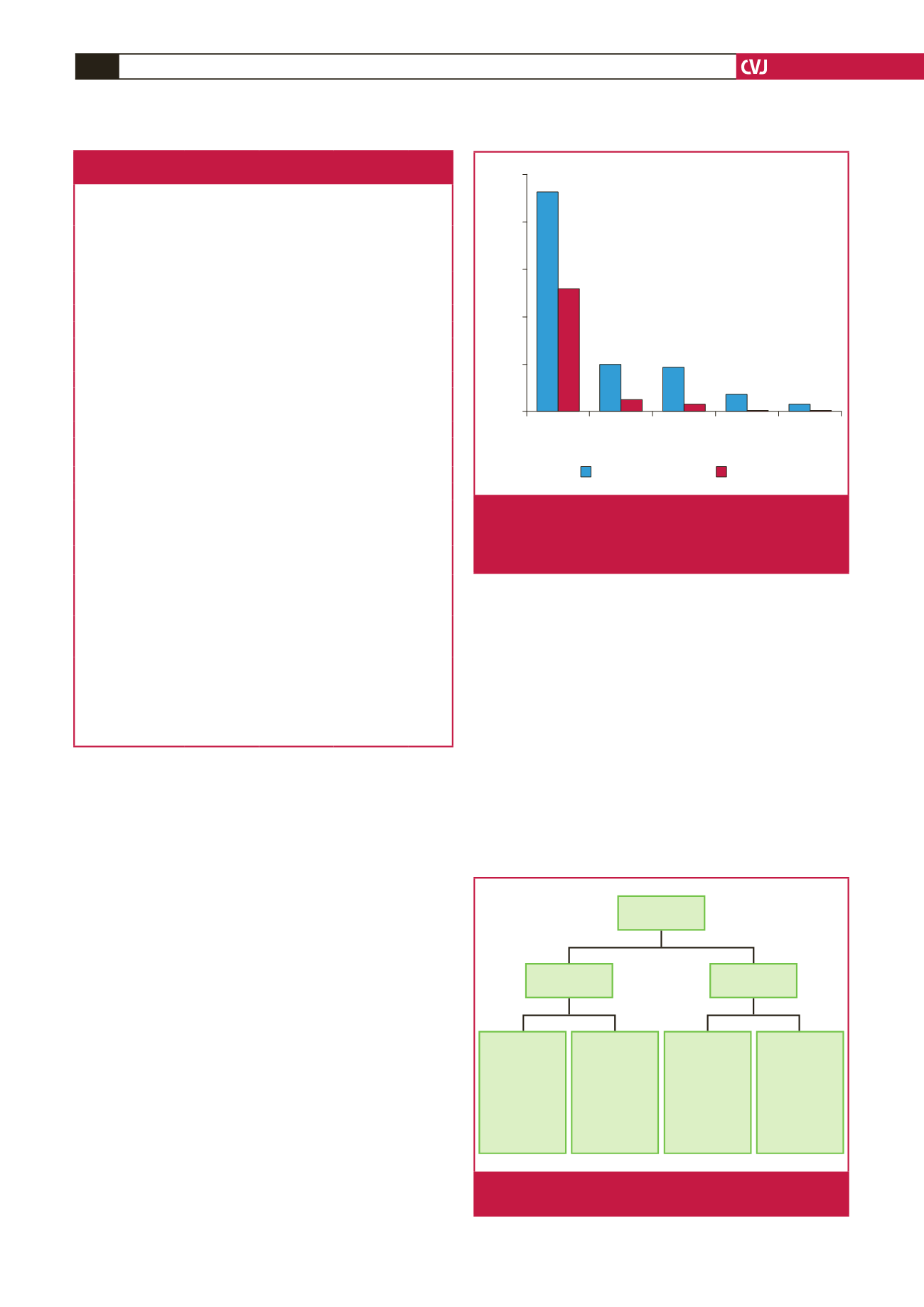
Fig. 1.
Time to complete closure. Only PDAs in which closure
was confirmed on echocardiography were included (
p
<
0.001 for the comparison between time to closure
with Amplazer and coils).
Multiple coils
(
n
=
18)
Coils
(
n
=
92)
Single coil
(
n
=
74)
Unsuccessful
(
n
=
5)
Surgery: 2
Lost to follow
up: 1
Closed
spontaneously: 1
Tiny residual
PDA: 1
Deployed
(
n
=
69)
Closed: 51
Repeat cath: 8
(2 unknown
result, 6 closed)
Residual flow: 4
Lost to follow
up: 6
Unsuccessful
(
n
=
6)
Surgical closure:
4
Repeat cath: 1
Lost to follow
up: 1
Deployed
(
n
=
12)
Closed: 12
Fig. 2.
Flow chart describing the patients who had PDA
closure with coiling.

















