
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 4, July/August 2018
252
AFRICA
Review Article
The challenge in diagnosing coarctation of the aorta
Julien IE Hoffman
Abstract
Critical coarctation of the aorta in neonates is a common
cause of shock and death. It may be the most difficult of all
forms of critical congenital heart disease to diagnose because
the obstruction from the coarctation does not appear until
several days after birth (and after discharge from the hospi-
tal), and because there are no characteristic murmurs. Some
of these patients may be detected by neonatal screening by
pulse oximetry, but only a minority is so diagnosed. Older
patients are usually asymptomatic but, although clinical diag-
nosis is easy, they are frequently undiagnosed.
Keywords:
patent ductus arteriosus, left ventricular failure, pulse
oximetry, balloon dilatation, stent
Submitted 14/7/17, accepted 19/11/17
Published online 11/12/17
Cardiovasc J Afr
2018;
29
: 252–255
www.cvja.co.zaDOI: 10.5830/CVJA-2017-053
Coarctation of the aorta is a congenital lesion that occurs in 2.5
to four per 10 000 live births.
1,2
With a total world population
of 7.5
×
10
9
and an annual crude birth rate of about 1.365
×
10
6
, each year about 340 000 to 550 000 children are born with
coarctation of the aorta. The anomaly is usually sporadic and is
more frequent in males.
Most coarctations fall into one of two groups: critical
coarctation of the aorta that causes symptoms within two
months of birth and if untreated causes death, and asymptomatic
coarctation of the aorta that presents later, usually with
hypertension in the upper limbs. Critical coarctation of the aorta
accounts for about 60% of all coarctations.
Pathological anatomy
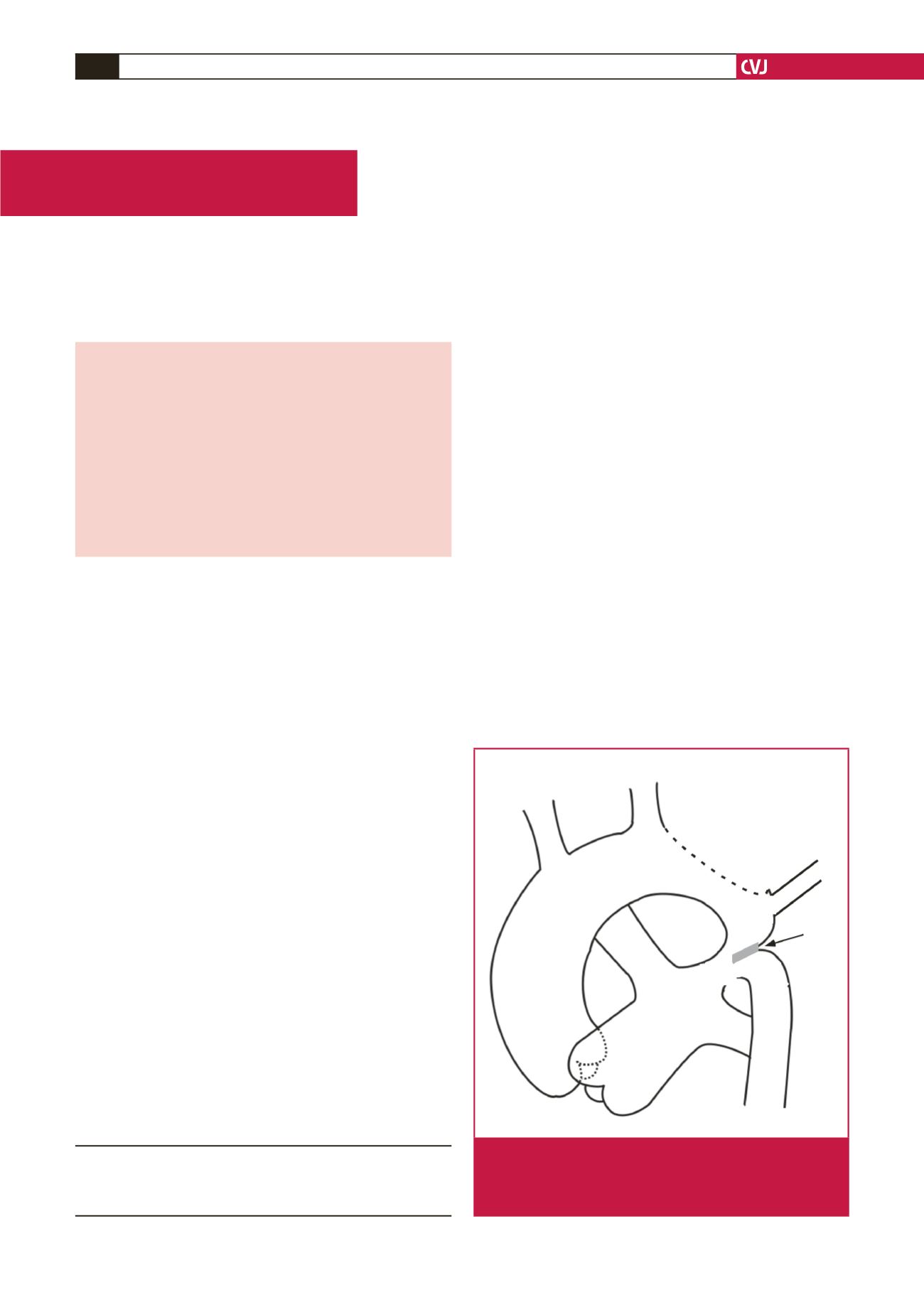
Anatomically a coarctation of the aorta is a shelf of tissue
extending from the postero-lateral aortic wall towards the ductus
arteriosus (Fig. 1). The shelf is near the patent ductus arteriosus,
sometimes above or below it, and is better termed juxtaductal. A
sling of ductus muscle passes around the shelf, and more ductus
muscle extends into the aortic wall above and below the shelf.
This is important, because unlike most other smooth muscle,
ductus smooth muscle tends to contract when exposed to high
oxygen concentrations.
The arch is often hypoplastic and when present, an associated
intracardiac shunt should be suspected. Most commonly this
is an isolated ventricular septal defect, but almost any form
of complex congenital heart disease can be associated. About
50 to 70% of the patients have a bicuspid aortic valve. The left
subclavian artery is often hypoplastic, and in approximately 5%
of these patients arises distal to the shelf.
Developmental physiology
In the foetus, the patency of the ductus arteriosus depends on
a balance between constrictors and dilators. Constriction is due
mainly to an increased sensitivity of ductus smooth muscle to
calcium
3
but also to endothelin. By contrast, the ductus smooth
muscle is relaxed by vasodilator prostaglandins (mainly PGE
2
)
that are produced in the ductus wall and also circulate from
the placenta.
4
The PGE
2
increases intracellular concentrations
of cAMP, which decreases calcium sensitivity. Nitric oxide and
Department of Pediatrics, University of California, San
Francisco, CA, USA
Julien IE Hoffman, MD,
jiehoffman@gmail.comIA
LCA
PDA
PA
LSA
Ductus
sling
Hypoplastic
arch
Asc aorta
Fig. 1.
Basic anatomy of coarctation of the aorta.Asc: ascend-
ing; IA: innominate artery; LCA: left carotid artery; LSA:
left subclavian artery; PA: main pulmonary artery;
PDA: patent ductus arteriosus.

















