
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 29, No 4, July/August 2018
AFRICA
249
A total of 49 Amplatzer™ devices were used in 46 patients.
Three devices were used during the study period: Amplatzer™
duct occluder 1 (37 patients), Amplatzer™ vascular plug (eight
patients), and one patient had an Amplatzer™ duct occluder 2
placed, a device that became available only towards the end of
the study period. Closure occurred in 93% of cases where an
Amplatzer™ device was used (43/46). In two instances, surgical
closure was required and in one patient a tiny residual PDA was
present that did not require closure.
Two patients with Amplatzer™ devices required another
catheterisation. In the first, an AVP was placed and there was a
tiny residual shunt. We attempted to place a coil inside the AVP,
which was unsuccessful, but as the residual PDA was very small
and insignificant, no further intervention was undertaken. In the
other patient, there was a gradient in the ADO pre-release, so the
device was removed and the procedure was abandoned. It was
later successfully closed with a smaller device.
Once Amplatzer™ devices became available at the facility, they
rapidly became the preferred device, with the drop in number of
coils used mirroring the increase in use of Amplatzer™ devices.
The number of patients who had a repeat procedure decreased
steadily over the 15 years, except for a brief period where repeat
procedures increased around the time the Amplatzer™ device was
introduced (Fig. 3). Lastly, the number of patients having their
PDA surgically ligated decreased several-fold over the 15-year
period (Fig. 4). The age of the child at surgical closure of the PDA
also reduced over time, from one year 10 months (1993–1997), to
nine months (1998–2002) and then seven months (2003–2008).
Minor complications were noted in 20% of patients (29/145)
(Table 3). A total of eight devices embolised (seven coils and one
Amplatzer device). None of these resulted in any permanent
problems. No differences were detected in the occurrence of
either minor or major complications related to the PDA shape.
Three major complications occurred (2%), all of which
resolved. In the first instance, a significant left pulmonary
artery obstruction was noted post PDA occlusion. The patient
was sent for surgery, the PDA was ligated and the device was
removed. The second patient developed complete heart block
during the procedure when the balloon on an Arrow–Berman™
catheter burst. Atropine was administered, supraventricular
tachycardia followed, which did not respond to adenosine, but
following DC cardioversion, sinus rhythm resumed. The PDA
was then successfully closed. The third patient had unusual PDA
anatomy with a Kommerell diverticulum. The PDA was closed
successfully, but on a cardiothoracic angiogram done after the
closure, a vascular ring was noted.
Recent experience with transcatheter closure
From January 2008 to August 2017, a total of 162 procedures
were performed at the facility for transcatheter occlusion of
PDA. These were predominately done with Amplatzer devices
(101 ADO1, 10 ADO2, 14 AVP2 and 6 ADO additional sizes).
An additional 22 cases were done with the Occlutech (Occ
Duct Occluder devices) and only two with coils. In four cases,
the device was removed and replaced during the transcatheter
procedure. In total, there were 10 procedures where a device
failed. In eight of these cases, the device was removed and the
patient then had a surgical procedure, and in the remaining two
cases, the device embolised. One was removed in the catheter
Table 3. Details of minor complications
Minor complications
Number Details
General
LV dysfunction
8
6 resolved, 2 lost to follow up
Diminished leg perfusion
2
Resolved with heparin infusion
Arrhythmia
3
SVT – reverted to sinus easily
1 – adenosine
2 – stimulation of RA with catheter
Haemolysis
1
Lost to follow up
Embolisation
Coils
7
(6 patients)
5 coils (4 patients) left
in situ
– no
long-term problems
2 coils removed by snares
Amplatzer
1
Removed percutaneously
Obstruction and site
Aorta (
n
=
2)
Coil
1
Mild gradient, observed, left
in situ
Amplatzer
1
Removed, smaller device used
Pulmonary arteries (
n
=
6)
Coil
1
Coil removed
Amplatzer
5
Mild gradient noted, not significant.
Devices left
in situ
Total
29/145 (20%)
SVT: supraventricular tachycardia.
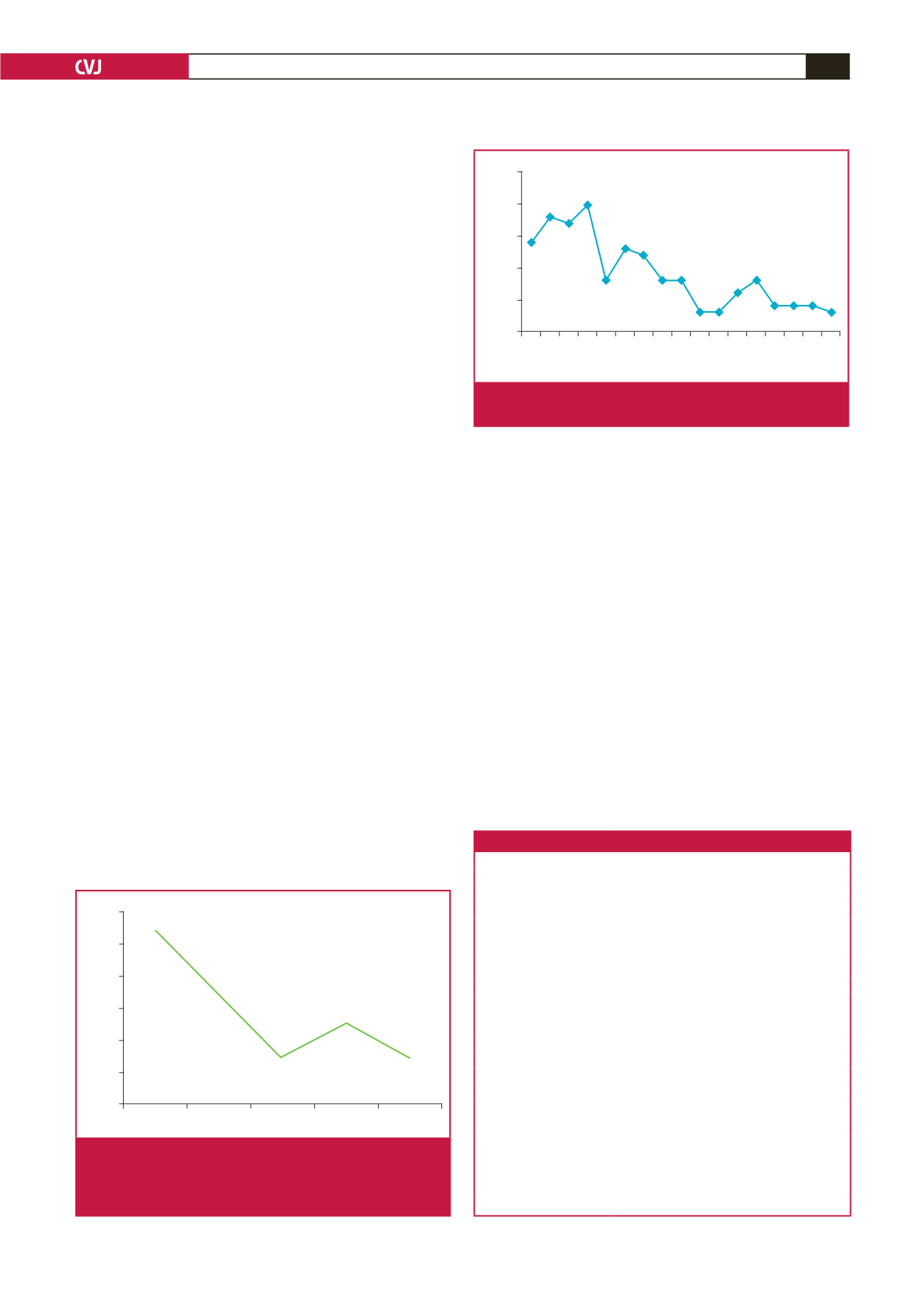
12
10
8
6
4
2
0
Number of patients
1994–1996 1997–1999 2000–2002 2003–2005 2005–2008
Fig. 3.
Number of patients requiring a repeat procedure to
close the PDA. This graph includes patients who
initially had surgery and then went for transcatheter
closure.
Number of PDAs
25
20
15
10
5
0
1992
2000
1996
2004
1994
2002
1998
2006
1993
2001
1997
2005
1995
2003
1999
2007
2008
Fig. 4.
Number of PDAs surgically ligated per year over the
study period.

















