
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 4, July/August 2017
226
AFRICA
The high HIV burden in South Africa and the known
prothrombotic nature of HIV has sensitised clinicians to
investigate HIV-infected patients with respiratory symptoms for
PE. The non-specific signs of PE, as well as the added TB disease
burden often confounds the clinical scenario in these patients
and probably results in more patients being imaged.
As the prevalence of HIV increases globally, the trend
towards increased CTPA imaging may result in higher incidence
rates of PE. This is yet to be proven by new studies undertaken
in this decade.
Prevalence of HIV in patients with PE
Major studies published to date have evaluated the relationship
between VTE and HIV by determining the frequency of PE in
HIV-positive hospital populations. Our study differs in that it
examined a population of patients with suspected PE who had
CTPA, and then determined the HIV prevalence in the whole
group as well as in those with proven PE.
More than two-thirds (68%) of the population undergoing
CTPA who were tested for HIV was shown to be infected. This
is the first study, performed at a local South African hospital, to
report on the prevalence of HIV in patients referred for CTPA
with confirmed PE (67%). This increased prevalence reflects the
population demographics of this hospital, which is known to have
the highest HIV burden locally in the Cape metropolitan area,
14
and
is therefore also reflective of the high clinical index of suspicion of
PE in HIV-positive patients presenting to this hospital.
No statistical significance was found in the prevalence of HIV
in patients with and without proven PE. This can be explained by
our small sample size, as there were insufficient data to suggest
a statistically significant association. The known association,
however, has already been proven by larger studies conducted
worldwide.
Pulmonary embolism and TB
Published studies evaluating the relationship between PE and TB
are limited and report the prevalence of VTE in TB populations.
Our study differs in that it determined the TB prevalence in
patients who underwent CTPA for suspected PE, and those with
proven PE.
Forty per cent of patients undergoing CTPA, who were tested
for TB, had microbiological confirmation of TB. We found a
statistically significant association (at the 10% level) between TB
positivity and PE. Additional randomised studies are however
required to confirm a positive association between PE and TB, as
we evaluated only patients with an available TB laboratory result.
Pulmonary embolism and the influence of TB in HIV
We further evaluated the HIV-positive group with confirmed PE
on CTPA to determine the prevalence of TB co-morbidity. We
found an overall 71% prevalence of TB in HIV-positive patients
with proven PE. No statistically significant difference however was
found in the prevalence of TB co-morbidity between HIV-positive
and -negative groups with identified PE. This prevalence was
much higher than the 47% rate of TB infection in HIV-positive
patients who developed DVT during their hospital admissions,
reported previously by Govender
et al
., in South Africa.
15
There is no agreement in the literature as yet as to whether
antiretroviral therapy has a progressive or additive effect
in promoting VTE. Some studies have implicated protease
inhibitors in VTE, while other studies showed no association.
8,16
Only 50% of our patients who were HIV infected and had
PE were on HAART regimens at any time during or prior to the
study. These numbers did not allow for evaluation of the effects of
HAART on severity and extent of PE. Further studies are required
to examine the effects of HAART regimens on VTE severity.
Distribution and severity of PE
No studies in the literature have compared detailed imaging
data with regard to CTPA findings between HIV-positive
and -negative patients. We demonstrated that in HIV-positive
patients, thrombi were most frequently found in the right (82%)
and left lower lobes (86%) of the lung. In the HIV-negative
patients, the most commonly affected lobe of the lung was the
left lower lobe (91%). No statistical difference was, however,
demonstrated in the prevalence of PE between the HIV-infected
and uninfected groups performed per lobe of the lung.
In evaluating the degree of occlusion in the different lobar
arteries/most proximal segments giving origin to the distal
segmental arteries of the lung, we found more extensive PE
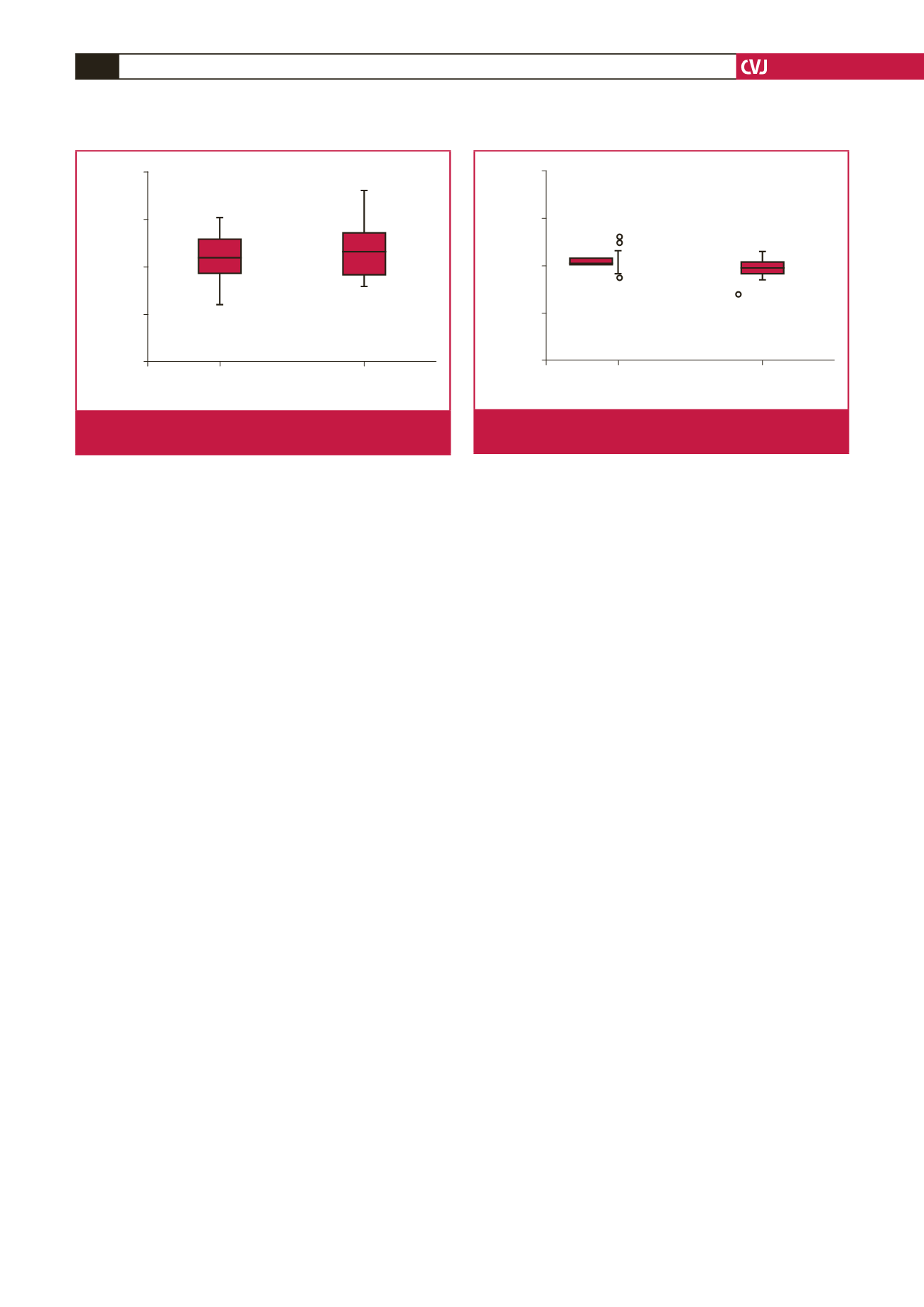
HIV status
HIV positive
HIV negative
VI/LV ratio
2.00
1.50
1.00
0.50
0.00
Fig. 6.
Differences between HIV positive and negative
according to RV:LV ratios (
p
=
0.611).
HIV status
HIV positive
HIV negative
PA/AO ratio
2.00
1.50
1.00
0.50
0.00
103
21 61
15
80
18
*
*
Fig. 7.
Differences between HIV positive and negative accord-
ing to PA:AO ratios (
p
=
0.191).

















