
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 6, November/December 2017
352
AFRICA
For each model, response options for the dependent
variable were categorised as either ‘poor adherence’ or ‘optimal
adherence’. The predictor variables were categorised as follows:
(1) gender: males and females; (2) age: 18–39 years, 40–49 years,
50–59 years, ≥ 60 years; (3) marital status: married and single
(includes divorced and widowed); (4) level of education: low–
intermediate (0–12 years) for those who completed secondary
school or less, and high (
>
12 years) for those who had a diploma,
bachelor degree or postgraduate degree; (5) residence: Khartoum,
Khartoum North, Omdurman and outside Khartoum State; (6)
hospitals: Ahmed Gasim Hospital, Elshaab Teaching Hospital
and Sudan Heart Institute; (7) monthly income: low
<
1 000
Sudanese pounds (SP), middle 1 000–2 000 SP, and high
>
2 000
SP; (8) number of chronic diseases: one to two chronic diseases,
and ≥ three chronic diseases; (9) number of medications taken:
one to four medications, and ≥ five medications); (10) duration
of medication use:
>
three months to one year,
>
one to five
years,
>
five to 10 years, and
>
10 years.
Results
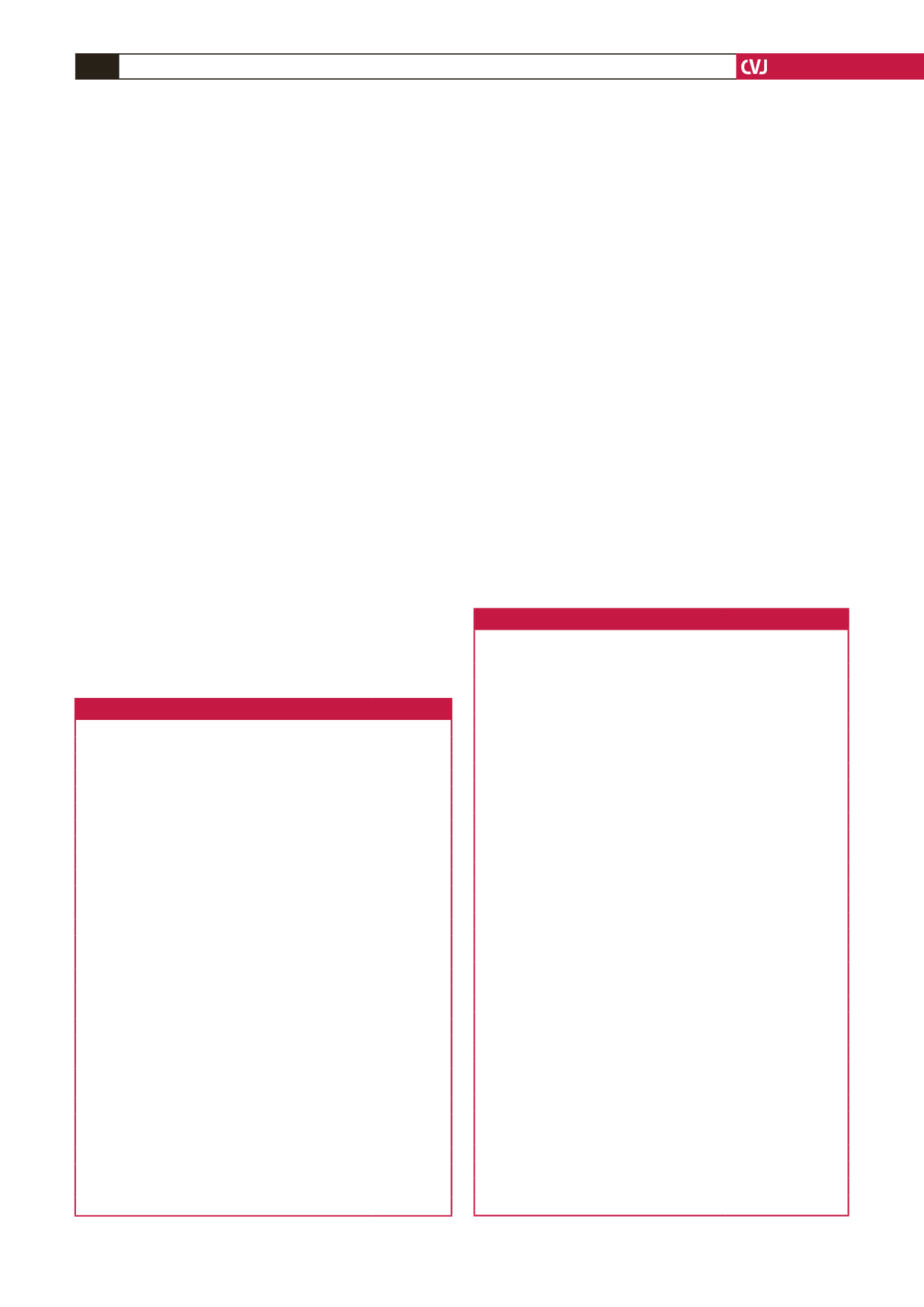
Table 1 summarises the sociodemographic characteristics of
respondents. A total of 433 Sudanese subjects were approached
to be included in the study; 386 agreed to participate, giving a
response rate of 89.1%. Of the respondents, 43% were 60 years
or over, 57% were females and 81.6% had low–intermediate
education.
Table 2 shows the clinical characteristics of the study
participants. One-half of respondents had hypertension, 30.3%
had dyslipidaemia and 28.5% had ischaemic heart disease. The
mean (
±
SD) number of chronic diseases among the study
population was 2.3 (
±
1.3) and that of medication use was 4.2
(
±
1.9). Two hundred and thirty-six patients (61.1%) were using
beta-blockers, and above two-fifths were using loop diuretics
(47.2%), statins (47.4%), low-dose aspirin (42.7%) and warfarin
(40.7%). The mean (
±
SD) duration of medication use among
participants was 6.4 (
±
5.4) years.
Table 3 presents the distribution of responses to the MMAS-
8 among the participants. Seven in 10 participants (
n
=
274;
71.0%; 95% CI: 66.1–75.4) reported that they never or rarely
had difficulty remembering to take all their medications. Half of
the respondents indicated that they felt hassled about sticking to
their treatment plan (
n
=
194; 50.3%; 95% CI: 45.2–55.4). Over
one-third of the study population reported that they had cut
back or stopped their medication without telling their physicians
because they felt worse (
n
=
140; 36.3; 95% CI: 31.5–41.3) and
that they sometimes forgot to take their pills (
n
=
133; 34.5; 95%
CI: 29.8–39.5).
Optimal adherence was defined as having a score of greater
than six on the MMAS-8. Using this cut-off point, 49% (
n
=
189; 95% CI: 43.9–54.1) of respondents had optimal medication
adherence and 51% (
n
=
197; 95% CI: 45.9–56.1) had poor
medication adherence. The mean (
±
SD) score for the medication
Table 1. Sociodemographic characteristics of the respondents (
n
=
386)
Characteristic
Frequency (%)
Gender
Male
166 (43)
Female
220 (57)
Marital status
Single*
239 (61.9)
Married
147 (38.1)
Age (years)
18–39
79 (20.5)
40–59
42 (10.9)
50–59
99 (25.6)
≥ 60
166 (43.0)
Educational level
Low–intermediate education
315 (81.6)
High education
71 (18.4)
Residence (cities in Khartoum State)
Khartoum
75 (19.4)
Khartoum North
102 (26.4)
Omdurman
92 (23.8)
Outside Khartoum State
117 (30.3)
Hospitals
Ahmed Gasim Cardiac Surgery and Renal
Transplantation Centre
110 (28.5)
Elshaab Teaching Hospital
146 (37.8)
Sudan Heart Institute
130 (33.7)
Monthly income
Low income
140 (36.3)
Middle income
136 (35.2)
High income
110 (28.5)
*Includes divorced and widowed
Table 2. Clinical characteristics of the respondents (
n
=
386)
Characteristic
Frequency (%; 95% CI)
Types of chronic diseases
Hypertension
195 (50.5; 45.42–55.6)
Dyslipidaemia
117 (30.3; 25.8–35.2)
Ischaemic heart disease
110 (28.5; 24.1–33.3)
Chronic heart failure
85 (22.0; 18.1–26.6)
Arrhythmia
81 (21.0; 17.1–25.5)
Cardiac valve replacement
74 (19.2; 15.4–23.5)
Rheumatic heart disease
71 (18.4; 14.7–22.7)
Cerebrovascular disease
25 (6.5; 4.3–9.5)
Drug class/drug
Beta-blockers
236 (61.1; 56.1–66.0)
Statins
183 (47.4; 42.4–52.5)
Furosemide
182 (47.2; 42.1–52.3)
Low-dose aspirin
165 (42.7; 37.8–47.9)
Warfarin
157 (40.7; 35.8–45.8)
Angiotensin converting enzyme inhibitors
147 (38.1; 33.3–43.2)
Potassium-sparing diuretics
115 (29.8; 25.3–34.7)
Calcium-channel blockers
63 (16.3; 12.9–20.5)
Clopidogrel
60 (15.5; 12.2–19.6)
Angiotensin receptor blockers
48 (12.4; 9.4–16.2)
Nitrates
44 (11.4; 8.5–15.1)
Digoxin
31 (8.0; 5.6–11.3)
Thiazide diuretic
15 (3.9; 2.3–6.5)
Number of chronic diseases
1–2
234 (60.6; 55.5–65.5)
≥ 3
152 (39.4; 34.5–44.5)
Number of medications
1–4
216 (56.0; 50.8–61.0)
≥ 5
170 (44.0; 39.1–49.2)
Duration of medication use (years)
≥ 0.25–1
75 (19.4; 15.7–23.8)
>
1–5
143 (37.0; 32.3–42.1)
>
5–10
95 (24.6; 20.5–29.3)
>
10
73 (18.9; 15.7–23.8)

















