
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 6, November/December 2017
AFRICA
357
erythrocyte sedimentation rate and lactate dehydrogenase
enzyme (LDH) levels.
•
Arterial gasometry: presence of hypoxaemia, acute respira-
tory alkalosis and changes not related to PE.
•
Chest X-ray: presence of atelectasis, parenchymal infiltrates,
pleural effusion, pneumothorax, cardiomegaly, Westmark
and Hampton signs and changes not related to PE.
•
ECG: presence of sinus tachycardia, S1Q3T3 pattern, pulmo-
nary P wave, right bundle branch block, right ventricular
hypertrophy, right cardiac axis deviation, reversal of T wave
in V1–V3 leads and unspecific alterations of repolarisation.
•
Echocardiogram: presence of enlargement or thrombus in the
right chambers, right ventricle (RV) hypokinesia, McConnell
sign, persistent pulmonary hypertension, patent foramen
ovale and changes not related to PE.
•
Doppler ultrasound of limbs: presence of thrombi or
decreased venous compressibility.
•
Pulmonary computed tomography angiography (PCTA): the
lesions were classified as massive PE if the thrombosis was in
a central location (main and lobar branches); patients with
thrombosis in the segmental and sub-segmental branches
were classified as sub-massive PE if RV dysfunction was
present; and they were classified as low-risk PE on the
absence of thrombus.
Patients were also classified as haemodynamically unstable if
their systolic blood pressure was under 90 mmHg, or there was
poor peripheral perfusion or cardiogenic shock, and according
to the pulmonary embolism severity index (PESI).
9
The treatment type and duration was analysed. The following
complications were considered: death; reversed cardiorespiratory
arrest; heart failure; respiratory failure requiring mechanical
ventilation; major bleeding, cardiogenic shock, acute myocardial
infarction, acute kidney injury (AKI) or chronic kidney
disease agudisation, sepsis originating in the respiratory tract,
hyperglycaemia
>
200 mg/dl (11.1 mmol/l) in non-diabetic
patients, and peripheral embolisation.
Data are presented using tables with absolute and relative
frequencies, average arithmetic values and standard deviations.
Statistical analysis was performed as two-sided significance
tests. The non-parametric chi-squared test was used to test
heterogeneity of proportions.
Results
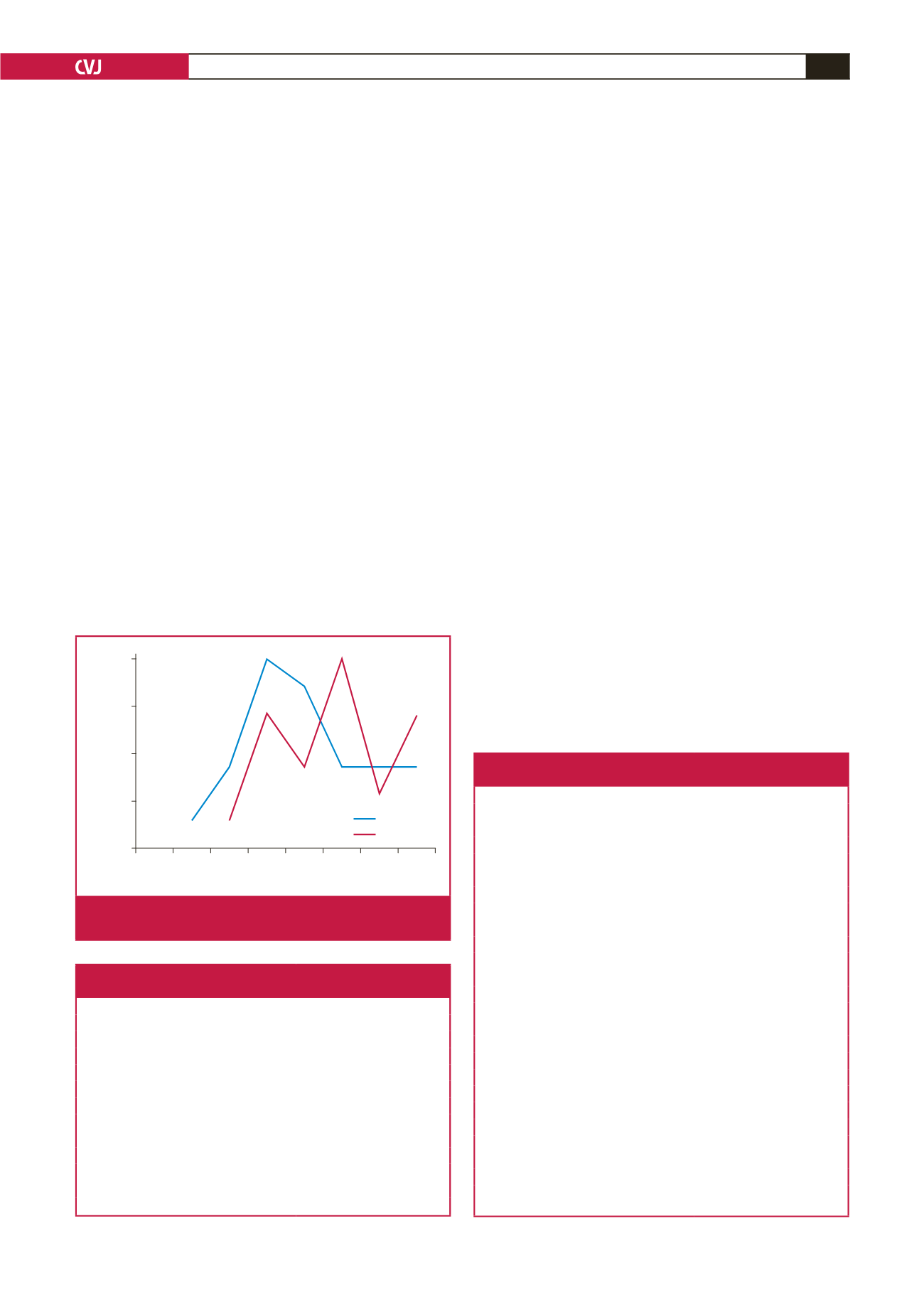
A total of 50 patients were included and the median age was 50.5
±
17.8 years. The age groups 35 to 44 years and 55 to 64 years
were the most affected (Fig. 1), 72% of patients were over the age
of 40 years, 52% were male and 86% were black.
Respiratory symptoms, including dyspnoea (68%), chest
pain (40%) and cough (18%) were the most frequent. Only 4%
of patients were asymptomatic and one patient presented with
cardiorespiratory arrest (Table 1).
Risk factors and more prevalent co-morbidities were
immobilisation for more than 72 hours (48%), hospitalisation or
recent surgery (28%), and hypertension (36%). In three patients
(6%) there were no identified risk factors or co-morbidities
(Table 2).
The estimated pre-test probability of PE was analysed
according to the Wells and Geneva criteria. Fifty-six and 58%
Table 1. Prevalence of symptoms and signs of patients
with pulmonary embolism at admission
Symptoms and signs
Number (%)
Dyspnoea
34 (68)
Chest pain
20 (40)
Cough
9 (18)
Lower-limb pain
7 (14)
Tachycardia
6 (12)
Altered consciousness
5 (10)
Anxiety
3 (6)
Cyanosis
1 (2)
Syncope
1 (2)
Cardiorespiratory arrest
1 (2)
Other symptoms
15 (30)
Asymptomatic
2 (4)
Table 2. Risk factors and co-morbidities of patients
with pulmonary embolism
Risk factors and co-morbidities
PE,
n
(%)
Immobilisation
>
72 hours
24 (48)
Hospitalisation/surgery < 3 months
14 (28)
Arterial hypertension
18 (36)
Recent trauma
8 (16)
Diabetes mellitus
6 (12)
Obesity
6 (12)
Cancer
5 (10)
Previous known coagulations disorders
4 (8)
Smoking
4 (8)
Coronary artery disease/previous AMI
3 (6)
Hormonal treatment
3 (6)
Deep-vein thrombosis
3 (6)
Dyslipidaemia
2 (4)
Heart failure
2 (4)
COPD
1 (2)
Previous PE < 3 months
1 (2)
Stroke
1 (2)
Sickle cell disease
1 (2)
Pregnancy
1 (2)
Central venous catheter
1 (2)
Atrial fibrilation
1 (2)
Chronic kidney disease
1 (2)
No risk factors or co-morbidities
3 (6)
AMI, acute myocardial infarction; COPD, chronic obstructive pulmonary
disease.
Age
Male
Female
<18 18–24 25–34 35–44 45–54 55–64 65–74 75–84
No of patients
7
5
4
2
0
Fig. 1.
Age and gender of the patients with pulmonary embo-
lism.

















