
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 5, September/October 2020
AFRICA
255
years compared to 5.2% in those 75 years or older.
16
In another
study in 1 470 NSTEMI patients from the Taiwan nationwide
registry, older age
≥
75 years increased mortality rate 4.9 times
compared to patients 45–64 years of age.
17
Our study represents the high risk elderly patients admitted
with a diagnosis of ACS face in a contemporary cardiology
clinic. About 71% of our patients were characterised by a
GRACE risk score higher than 150, and more than 70% had a LV
ejection fraction lower than 50%. As a treatment strategy, about
60% of our patients were managed invasively. In the literature,
angiography rate in this population was slightly lower than in our
study. In European and US registries, the reported proportion of
elderly patients assigned to an invasive strategy was 50 to 33% in
patients aged beyond 70 and 80 years, respectively.
15
Our analysis of elderly patients with ACS demonstrated that
an invasive strategy was associated with a lower mortality rate at
follow up of a maximum of 61 months in comparison with an
initial conservative strategy. Almost twice the risk of mortality
has been seen with the conservative strategy. Similar to our
results, Tegn
et al
. reported in their After Eighty study, an open-
label, multicentre study targeting NSTEMI patients older than
80 years, that an invasive strategy was superior to a conservative
strategy in reduction of composite events of death, myocardial
infarction, stroke and the need for urgent revascularisation (40.6
vs 61.4%, hazard ratio 0.53, 95% CI: 0.41–0.69;
p
=
0.0001) at a
median follow up of 1.53 years.
18
However in another study from
Saudi Arabia, PCI had no effect on mortality rate in elderly
patients with ACS.
19
During the follow-up period, 75% of the STEMI patients
in our study died. This value was 32% in the NSTEMI/USAP
patients. This shows that STEMI has a worse prognosis than
other types of ACS in elderly patients. Similar to our results, in
another study, it was shown that STEMI increased mortality risk
about two-fold compared to NSTEMI at older ages.
20
In another
study from Switzerland from 2001 to 2012, in-hospital mortality
rate decreased and PCI use was significantly increased in older
patients.
21
Ischaemic heart disease is the leading cause of death globally.
22
Because of the growth of the elderly population, the World
Health Organisation predicts that coronary heart disease deaths
will increase by 120 to 137% during the next two decades, and a
person aged over 80 years can expect about nine remaining years
of life.
23
For this reason, a strategy on how to treat very elderly
patients is essential. The results from the present study support
an invasive strategy in octogenarians presenting with ACS.
Our study has some limitations. First, it has a retrospective,
cross-sectional design with single-centre data. Due to
the retrospective retrieval of the patient data and the low
patient numbers, our study cannot be generalised to all elderly
populations. Second, diagnosis of ACS in the elderly population
is challenging and multiple co-factors may affect cardiac enzyme
elevation, so some patients could be misdiagnosed. Finally, the
presence of multiple co-morbidities and the frailty of patients
may affect long-term mortality rates in elderly patients.
Conclusion
Guideline-based therapy should be the basic strategy for all
age groups in the presence of ACS. Within the indications, an
invasive strategy should without doubt be applied in elderly
patients. Advanced age of the patient should not be the reason
for not receiving these treatments.
References
1.
Murray CJ, Lopez AD. Measuring the global burden of disease.
New
Eng J Med
2013;
369
(5): 448–457.
2.
Alexander KP, Newby LK, Cannon CP, Armstrong PW, Gibler WB,
Rich MW,
et al
. Acute coronary care in the elderly, part I.
Circulation
2007;
115
(19): 2549–2569.
3.
Montalescot G, Wiviott SD, Braunwald E, Murphy SA, Gibson CM,
McCabe CH,
et al
. Prasugrel compared with clopidogrel in patients
undergoing percutaneous coronary intervention for ST-elevation
myocardial infarction (TRITON-TIMI 38): double-blind, randomised
controlled trial.
Lancet
2009;
373
(9665): 723–731.
4.
Cannon CP, Harrington RA, James S, Ardissino D, Becker RC,
Emanuelsson H,
et al.
Comparison of ticagrelor with clopidogrel in
patients with a planned invasive strategy for acute coronary syndromes
(PLATO): a randomised double-blind study.
Lancet
2010;
375
(9711):
283–293.
5.
Roule V, Blanchart K, Humbert X, Legallois D, Lemaitre A, Milliez P,
et al
. Antithrombotic therapy for ACS in elderly patients.
Cardiovasc
Drugs Ther
2017: 1–10.
6.
Puymirat E, Aissaoui N, Cayla G, Lafont A, Riant E, Mennuni M,
et
al
. Changes in one-year mortality in elderly patients admitted with acute
myocardial infarction in relation with early management.
Am J Med
2017;
130
(5): 555–563.
7.
De Luca L, Olivari Z, Bolognese L, Lucci D, Gonzini L, Di Chiara A,
et al.
A decade of changes in clinical characteristics and management of
elderly patients with non-ST elevation myocardial infarction admitted in
Italian cardiac care units.
Open Heart
2014;
1
(1): e000148.
8.
De Luca L, Marini M, Gonzini L, Boccanelli A, Casella G, Chiarella F,
et al
. Contemporary trends and age‐specific sex differences in manage-
ment and outcome for patients with ST‐segment elevation myocardial
infarction.
J Am Heart Assoc
2016;
5
(12): e004202.
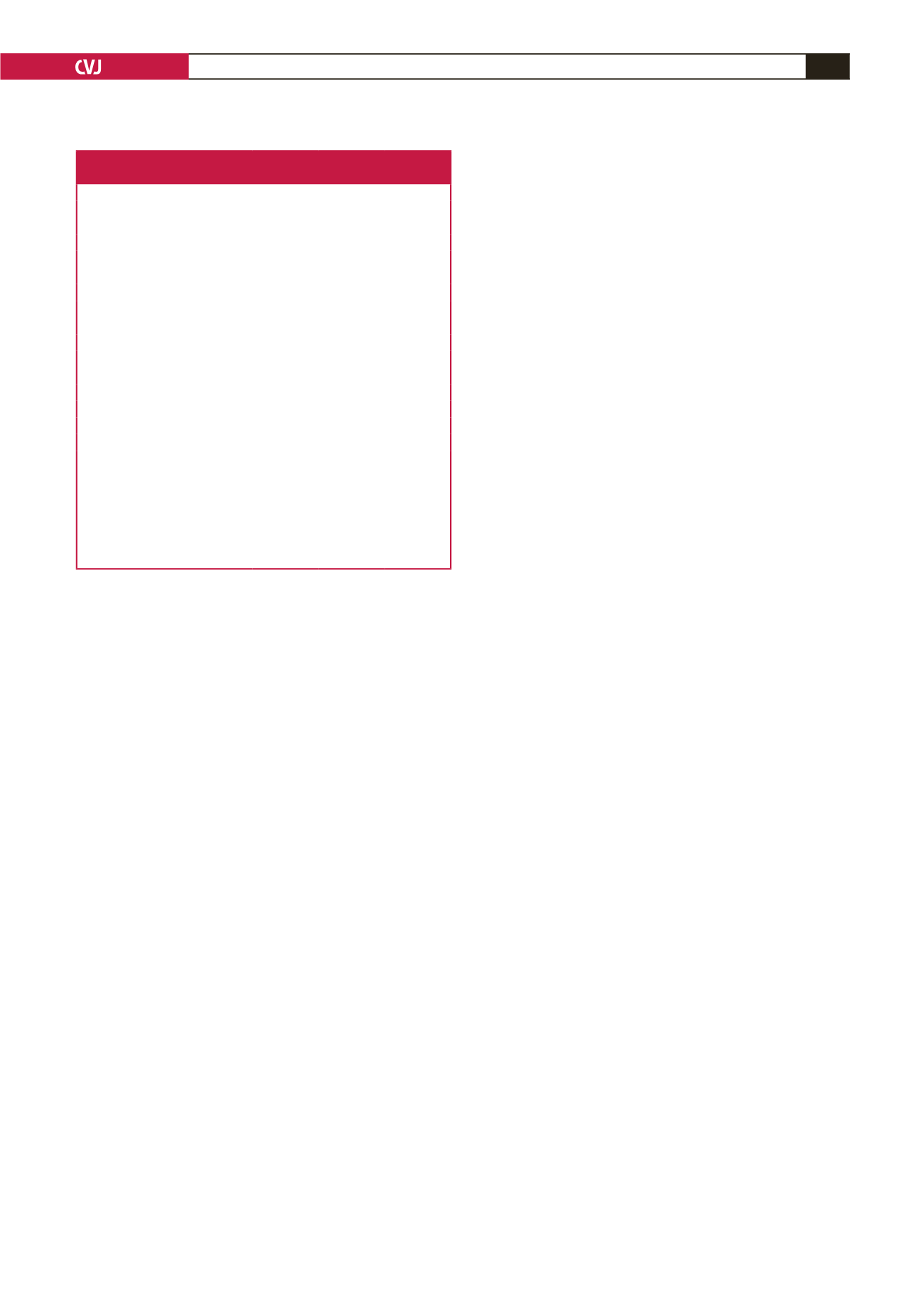
Table 3. Death predictors at the prespecified
by Cox multivariate analysis
Mortality
OR
95% CI
p
-value
Model 1
Invasive strategy*
Male
0.25
0.08–0.74
0.012
Hypertension
3.93
1.36–11.35
0.011
Ejection fraction
≤
40%***
2.65
1.11–6.32
0.027
GRACE risk score
4.49
1.66–12.10
0.003
<
150****
0.18
0.03–0.86
0.032
150–175****
0.32
0.10–0.96
0.043
ECG sinus rhythm
0.21
0.05–0.85
0.029
Model 2
Invasive strategy*
0.26
0.12–0.56
0.001
STEMI**
7.76
1.74–34.57
0.002
Ejection fraction
≤
40% ***
3.11
1.43–6.76
0.004
Heart rate (bpm)
0.98
0.96–0.99
0.013
GRACE risk score 150–175****
0.32
0.15–0.70
0.004
OR, odds ratio; CI, confidence interval.
*Conservative strategy as ref. **USAP as ref. ***Ejection fraction
>
40% as ref.
****Grace
>
175 as ref.
Model 1: Treatment protocols, gender, diabetes, hypertension, dyslipidaemia,
smoking, diagnosed, ejection fraction, ECG results, presentation symptoms,
GRACE risk score.
Model 2: Treatment protocols, diagnosed, ejection fraction, heart rate, ECG
results, smoking, admission SBP, presentation symptoms, GRACE risk score,
CKMB peak value, troponin peak value.



















