
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 5, September/October 2020
258
AFRICA
staffed by two general paediatricians with training in paediatric
echocardiography and cardiology.
The clinic screened referrals for cardiac disease and managed
children with known cardiac conditions, including CHD. Initial
assessment of patients included history, physical examination,
chest radiography and electrocardiography. Echocardiography
was performed at the discretion of the attending paediatrician if
any of the initial investigations suggested heart disease.
Patients diagnosed with CHD were managed medically,
with repeat clinic follow-up visits, including echocardiograms
as required. Patients requiring surgical correction were referred
to South Africa and, following post-surgery hospital discharge,
were managed back in Botswana.
Inclusion criteria were patients younger than 15 years of age
who were seen at the PMH paediatric cardiac clinic and who
had had at least one echocardiogram. Patients were identified
by reviewing clinic echocardiography reports and applying the
inclusion criteria. Duplicate records were deleted and only the
initial echocardiography report was retained. The list of data
points extracted included: age, gender, weight, and indication for
and result of the echocardiogram.
During data collection we noted that from May 2014,
all paediatric echocardiographs were performed by one
paediatrician. Given that this paediatrician’s record keeping
was good, all echocardiograph reports performed after May
2014 were available for analysis. This presented an excellent
opportunity to assess whether the spectrum of CHD that
had been sampled between 1 January 2010 and 31 December
2012 was similar to that seen in 2014. Hence we included a
comparator group for three months of 2014 (from 1 September
to 30 November 2014) to assess for possible sampling bias.
Statistical analysis
Data were summarised using standard descriptive statistics and
analysed using STATA version 12.0 (College Station, TX). A
p
-value of
<
0.05 was deemed significant.
To estimate the prevalence of CHD, we took two approaches:
first, for the three years from 2010 to 2012 with records from
a single paediatrician, we calculated the number of new CHD
patients seen per year. Given that this figure reflected the
echocardiography reports of one of two paediatric cardiologists,
we doubled this number to estimate the real number seen by two
paediatric cardiologists per year. Using Botswana’s 2012 annual
birth cohort of 40 856 from the Botswana Vital Statistics Report
as the denominator, we then estimated the prevalence of CHD.
For the comparator group, we used the same calculation
to estimate the prevalence of CHD: for three months of 2014,
we noted the number of unique patients with CHD. To adjust
for the fact that patients return every three to six months for
review at the clinic and that for these three months in 2014, the
paediatric cardiologist was not on leave, we multiplied this by
two to estimate the number of new unique CHD patients seen
in the year 2014. This number was then used as the numerator,
with the denominator the annual birth cohort, to estimate the
prevalence of CHD in 2014.
Results
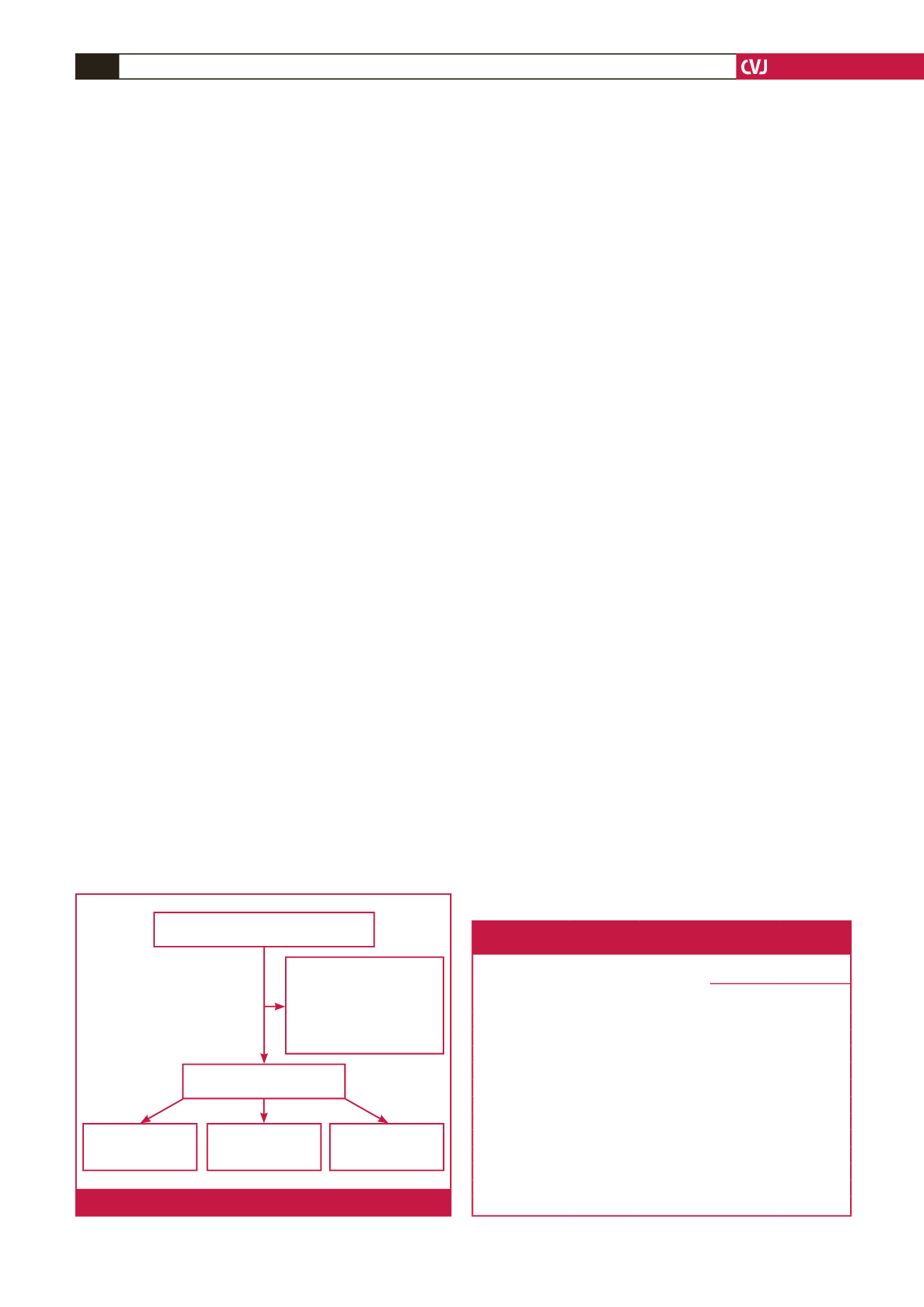
Overall, 377 subjectsmet study inclusion criteria (Fig. 1). Of these,
170 (45%) had CHD, 150 (40%) had normal echocardiographs
and 57 (15%) had acquired cardiac disease.
Demographics are summarised in Table 1. The median age of
the study population was 1.3 years (interquartile range 2 months
to 5.4 years) with a fairly even age distribution among children
with CHD, whereas children with acquired heart disease tended
to be in the oldest age group of 5 to 15 years (46%). Almost a
quarter (24%) of patients with CHD had a weight-for-age less
than the third standard deviation.
Indications for echocardiography are summarised in Table
2. The most common recorded indication was a known risk
factor for CHD, including trisomy 21 (
n
=
10, 11%) and other
dysmorphic features (
n
=
7, 7%). However, CHD risk factors
were not specified in the majority of patients.
The distribution of CHD types is summarised in Fig. 2.
The most common acyanotic congenital cardiac lesion was
ventricular septal defect (VSD) (50/170; 29%). The most common
cyanotic congenital cardiac lesion was tetralogy of Fallot (TOF)
(11/170; 6%).
Of the 50 VSDs, VSD type was recorded in 23 (46%) cases:
8/23 (35%) were muscular, 8/23 (35%) were membranous, 5/23
(22%) were outlet and 2/23 (9%) were inlet. VSD size was small
Total no of echocardiographs performed
during the study period = 393
Exclusions = 16:
Age > 15 years = 6
Unknown age = 7
Echocardiograph
prior to 2010 = 2
Unknown date of
echocardiograph = 4
Total no of participants
included in study = 377
No of patients with
normal echocardio-
graph = 150 (40%)
No of patients with
CHD = 170 (45%)
No of patients with
acquired lesions =
57 (15%)
Fig. 1.
Flow diagram of enrolled participants.
Table 1. Clinical characteristics of children with normal versus
abnormal echocardiographs
Whole study
population
(n
=
377) (%)
Normal
echocardio-
gram
(n
=
150) (%)
Abnormal echocardiogram
(n
=
227) (%)
CHD
(n
=
170) (%)
Acquired
(n
=
57) (%)
Male gender*
188 (50)
74 (49)
85 (50)
29 (51)
Age group
0–3 months
102 (27)
47 (31)
50 (28)
5 (9)
>
3 m–1 years
82 (22)
34 (23)
39 (23)
9 (11)
>
1–5 years
90 (24)
25 (17)
48 (28)
17 (30)
>
5–15 years
103 (27)
44 (29)
33 (19)
26 (46)
Weight for age
Normal (
>
0 SD)
80 (21)
36 (24)
34 (20)
10 (18)
0 to –3 SD
157 (42)
59 (39)
70 (41)
28 (49)
<
–3 SD
72 (19)
26 (17)
40 (24)
6 (11)
Unknown
68 (18)
29 (19)
26 (15)
13 (23)
*There were five patients with unknown gender, the rest were female (
n
=
184).



















