
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 4, July/August 2021
AFRICA
217
consumption (as reference) for the incidence of CVD events
reported in the included studies, we computed the log of RR and
the matching standard error for the overall pooled RR (95% CI)
for the incidence of CVD events and by subgroup stratification
[cerebral infarction, cerebral haemorrhage, coronary heart disease
(CHD), etc.] using an inverse-of-variance method for weighting
in all quantitative estimations for dichotomous outcomes.
The degree of heterogeneity was assessed using
I
2
statistics
assuming a fixed-effect model (where
I
2
< 50%) or a random-
effect meta-analysis model if
I
2
> 50%. The fixed-effect model
presupposes the effect size is likely relatively similar across
studies in the meta-analysis.
37,38
However, a random-effect model
ideates the difference in effect estimates across studies are valid
but follows a normal distribution. Publication bias for the likely
effect estimate of GLV intake on CVD events was tested using
funnel plots.
The constancy of the pooled RR (95% CI) was tested using
the leave-one-study-out method (carrying out the meta-analysis
several times, excluding a study at a time). All quantitative
analyses were conducted at
p < 0.05
using the RevMan 5.4
software.
39
Results
Over 3 000 records were retrieved from the literature search in
Google Scholar, EMBASE, MEDLINE, HINARI and Cochrane
Library but 1 021 duplicates were excluded. Also, 2 011 records
were excluded after screening the titles and abstracts (Fig. 1). On
full-text assessment, 65 records were excluded and 17 prospective
reports (five reports on composite CVD events,
10,25-27,40
five reports
on coronary heart disease,
28,41-44
one report on heart failure
45
and
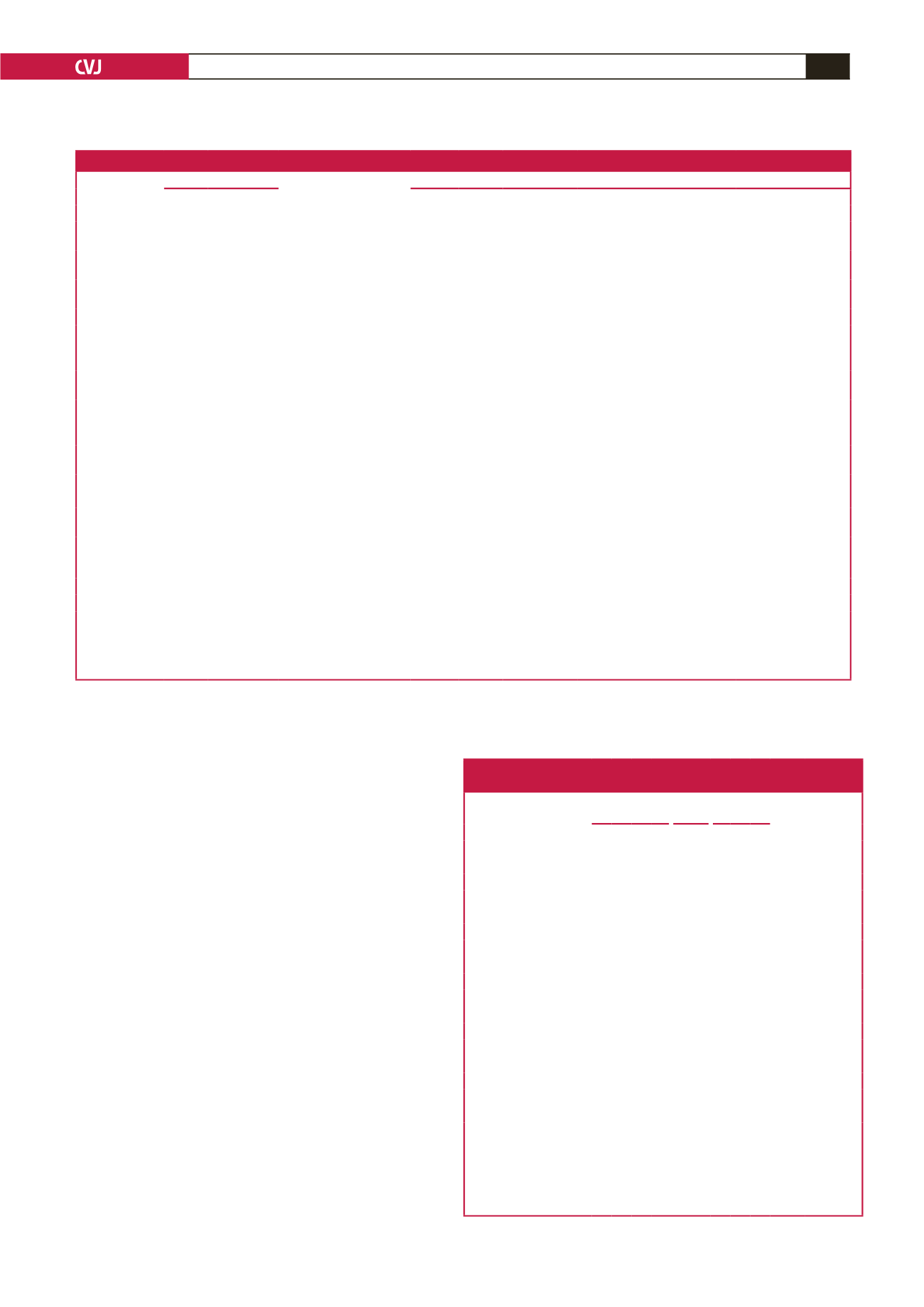
Table 1. Characteristics of prospective reports included in the meta-analysis
First author
Study characteristics
GLV intake
Baseline/outcomes evaluation
Year
Country
Incidence Total
CVD event(s)
Assessment
Ascertainment
Gaziano JM 1995 United States
< 1 s/d* vs ≥ 1 s/d
161 1 299
CVD
Relative-reported deaths
‡†
Not reported
Joshipura KJ
1999 United States
Increment of 1 s/d
3
366
W
204
M
75 596
W
38 683
M
Ischaemic
stroke
Self/relative report
‡
National Stroke Soci-
ety (NSS) criteria
Joshipura KJ
2001 United States
Increment of 1 s/d
2,3
1 127
W
1 063
M
84 251
W
42 148
M
CHD
Self/relative report
‡
World Health Organ-
isation (WHO) criteria
Johnsen SP
2003 Denmark
1.4 g/d* vs 28.00 g/d
266 54 506 Ischaemic
stroke
Self/relative report
‡
WHO criteria
Sauvaget C
2003
Japan
≤ 1 s/week* vs 1 s/d
2
1 926 40 349
Stroke
Stroke mortality
‡
WHO criteria
Hung HC
2004 United States
Increment of 1 s/d
3
3 864 109 635
CVD
Self/relative report
‡
NSS criteria
Takachi R
2007
Japan
Not reported
1 386 77 891
CVD MI or stroke diagnosis using CT
scan/MRI
‡
WHO and NSS
criteria
Joshipura KJ
2009 United States
Not reported
1 852
W
2 040
M
70 870
W
38 918
M
Ischaemic
CVD
Self/relative report
‡
WHO and NSS
criteria
Bendinelli B
2010
Italy
≤ 17.60 g/d* vs > 50.80 g/d
1
144 29 689
CHD
©
Self/relative report
‡
Minnesota Code
Oude Griep LM 2011A Netherlands
34 g/d* vs 105 g/d
2,3
233 20 069
Stroke
Population and hospital discharge
register
Dutch guidelines
Oude Griep LM 2011B Netherlands
34 g/d* vs 105 g/d
2,3
245 20 069
CHD
©
Population and hospital
discharge register
WHO criteria
Larsson S
2013
Sweden < 2.3 s/d* vs > 6.0 s/d
1,2,3
4 089 74 961
Stroke
Self report
‡
Not reported
Bhupathiraju SN 2013 United States 0.22 s/d* vs 1.50 s/day
1,2
6 189 71 141
CHD
Self/relative report
‡
WHO criteria
Rautiainen S
2015
Sweden
< 0.2 s/d* vs > 1 s/d
1,2,3
3 051 34 319 Heart failure Heart failure diagnosis and related
deaths
‡
ESC criteria
Wang JB
2016
China
Increment of twice/week 355 2 445
Stroke
Case, pathology, cytology, X-rays,
biochemical, ultrasound, endos-
copy and surgery reports
Team of reviewers
Buil-Cosiales P 2016
Spain
32·16 g/d* vs 113.00 g/d
1
342 7 216
CVD
Self/relative report
‡
Team of reviewers
Blekkenhorst LC 2017 Australia
Intake per 10 g/d
238 1 226
CHD CHD diagnosis and related death
‡
Not reported
*Reference group for comparison;
1
energy-adjusted dietary intakes of GLV;
2
additionally adjusted for other intakes, etc;
3
using median values of quintiles;
M
men;
W
wom-
en;
©
MI events, coronary revascularisation, or both not preceded by any other CHD event;
‡
authenticated via vital statistics or medical records or designated registry;
†
validated death certificate.
g/d – grams per day; s/d – servings per day; GLV – green leafy vegetables; ESC – European Society of Cardiology; CVD – cardiovascular disease; CHD – coronary heart
disease; CT – computed tomography; MI – myocardial infarction; MRI – magnetic resonance imaging.
Table 2. Methodological assessment of prospective studies
using the Newcastle–Ottawa scale
Study
Year
Selection
Compa-
rability Outcome Total
Scores
Risk of bias
of included
studies
S1 S2 S3 S4 C1 O1 O2 O3
Gaziano
et al
.
1995 1 1 1
1 1
1 6
High
Joshipura
et al.
1999 1 1 1 1 2 1 1 1 9
Low
Joshipura
et al.
2001 1 1 1 1 2
1 1 8 Moderate
Johnsen
et al
.
2003 1 1 1 1 2 1
1 8 Moderate
Sauvaget
et al.
2003 1 1
1 2 1 1 1 8 Moderate
Hung
et al
.
2004 1 1 1 1 2 1 1 1 9
Low
Takachi
et al.
2007 1 1 1
2 1
1 7 Moderate
Joshipura
et al.
2008 1 1 1 1 2
1 1 8 Moderate
Bendinelli
et al.
2010 1 1 1 1 2 1 1 1 9
Low
Oude
Griep et al.
2011A 1 1 1 1 2 1 1 1 9
Low
Oude Griep
et al.
2011B 1 1 1 1 2 1 1 1 9
Low
Larsson
et al
.
2013 1 1 1 1 2 1 1 1 9
Low
Bhupathiraju
et al
. 2013 1 1 1 1 2 1 1 1 9
Low
Rautiainen
et al.
2014 1 1 1 1 2 1 1 1 9
Low
Buil-Cosiales
et al
. 2016 1 1 1 1 2 1 1 1 9
Low
Wang
et al.
2016 1 1 1
2 1 1 1 8 Moderate
Blekkenhorst
et al.
2017 1 1 1 1 2 1 1 1 9
Low
Risk of bias of included studies: high risk of bias: ≤ 6; moderate risk of bias: 7–8;
low risk of bias: 9 and empty cells indicate a score of 0.
S1 – representativeness of the exposed cohort; S2 – selection of the non-exposed
cohort; S3 – ascertainment of exposure; S4 – demonstration that outcome of interest
was absent at the start of the study; C1 – comparability of the cohort based on the
design or analysis; O1 – assessment of outcome; O2 – was follow up long enough for
outcomes to occur?; O3 – adequacy of follow up of cohorts.



















