
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 4, July/August 2021
216
AFRICA
Apromising preventative strategy for CVD is diet.
10-13
However,
studies on the potential association of diet and CVD events have
focused on the effect of red meat,
14,15
salt intake,
16
alcohol,
17
saturated fats/oils and dairy products.
18
Prior reviews and meta-
analyses
19-24
investigating the effect of fruit and vegetables on the
risk profile for CVD have focused on broad categories of the
nutritional modalities. For example, Deng
et al.
19
and Kwok
et
al
.
24
in two reviews of meta-analyses assessed the effect of fruit
and vegetable intake, in general, on the burden of diseases and
all-cause mortality without providing information on the specific
effect(s) of green leafy vegetables (GLV) on the incidence of
distinct CVD events.
The information provided by individual studies on the
effect of GLV intake remains inconclusive. While some studies
reported a reduction in the incidence of CVD events with
higher consumption of GLV,
10,25,26
others observed statistically
insignificant relationships.
27,28
The pooled effect of GLV intake
on incident CVD is currently unknown.
GLV are widely available in LMIC.
29
The vegetables are rich
in phytochemicals and micronutrients known to be essential for
health.
13,30-32
Also, GLV contain folic acid, vitamins A, C, E and K,
as well as high amounts of calcium, iron, potassium, phosphorous
and zinc,
33,34
which may be protectively associated with CVD
risk.
35
This systematic review and meta-analysis investigated the
pooled effect of GLV intake on incident CVD events.
Methods
The systematic review was registered in the international
prospective register of systematic reviews and is accessible
via
https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020181050. Google Scholar, EMBASE,
MEDLINE, HINARI and Cochrane Library were searched
(in December 2020 using specific search terms independent
of language and publication dates) for previously published
epidemiological reports on consumption of GLV and CVD. The
following search terms were used.
EMBASE, Google Scholar and Cochrane Library search
terms: ‘vegetables’ OR ‘chlorophyll-containing vegetables’ OR
‘green leafy vegetables’ OR ‘broccoli’ OR ‘cabbage’ OR ‘celery’
OR ‘collard green’ OR ‘green pea’ OR ‘lettuce’ OR ‘spinach’ OR
‘swiss chard’ OR ‘turnip green’ AND ‘cardiovascular disease’ OR
‘cerebrovascular disease’ OR ‘cerebral infarction’ OR ‘cerebral
haemorrhage’ OR ‘coronary heart disease’ OR ‘heart failure’ OR
‘subarachnoid haemorrhage’.
MEDLINE and HINARI search terms using PubMed
interphases:
‘vegetables (Title/Abstract)’ OR ‘green leaves (Title/
Abstract)’ OR ‘edible green leaves (Title/Abstract)’ OR ‘green
vegetables (Title/Abstract)’ OR ‘leafy vegetables (Title/Abstract)’
OR ‘green leafy vegetables (Title/Abstract)’ OR ‘chlorophyll-
containing vegetables (Title/Abstract)’ OR ‘broccoli (Title/
Abstract)’ OR ‘cabbage (Title/Abstract)’ OR ‘celery (Title/
Abstract)’ OR ‘collard green (Title/Abstract)’ OR ‘green pea
(Title/Abstract)’ OR ‘lettuce (Title/Abstract)’ OR ‘spinach (Title/
Abstract)’ OR ‘swiss chard (Title/Abstract)’ OR ‘turnip green
(Title/Abstract)’ AND ‘stroke (MesH terms)’ OR ‘transient
ischemic attack (MeSH terms)’ OR ‘haemorrhagic stroke (MeSH
terms)’ OR ‘ischaemic stroke (MeSH terms)’ OR ‘cardiovascular
disease (MeSH terms)’ OR ‘cerebrovascular disease (MeSH
terms)’ OR ‘cerebral infarction (MeSH terms)’ OR ‘cerebral
haemorrhage (MeSH terms)’ OR ‘coronary heart disease (MeSH
terms)’ OR ‘heart failure (MeSH terms)’ OR ‘subarachnoid
haemorrhage (MeSH terms)’. Details of the literature search are
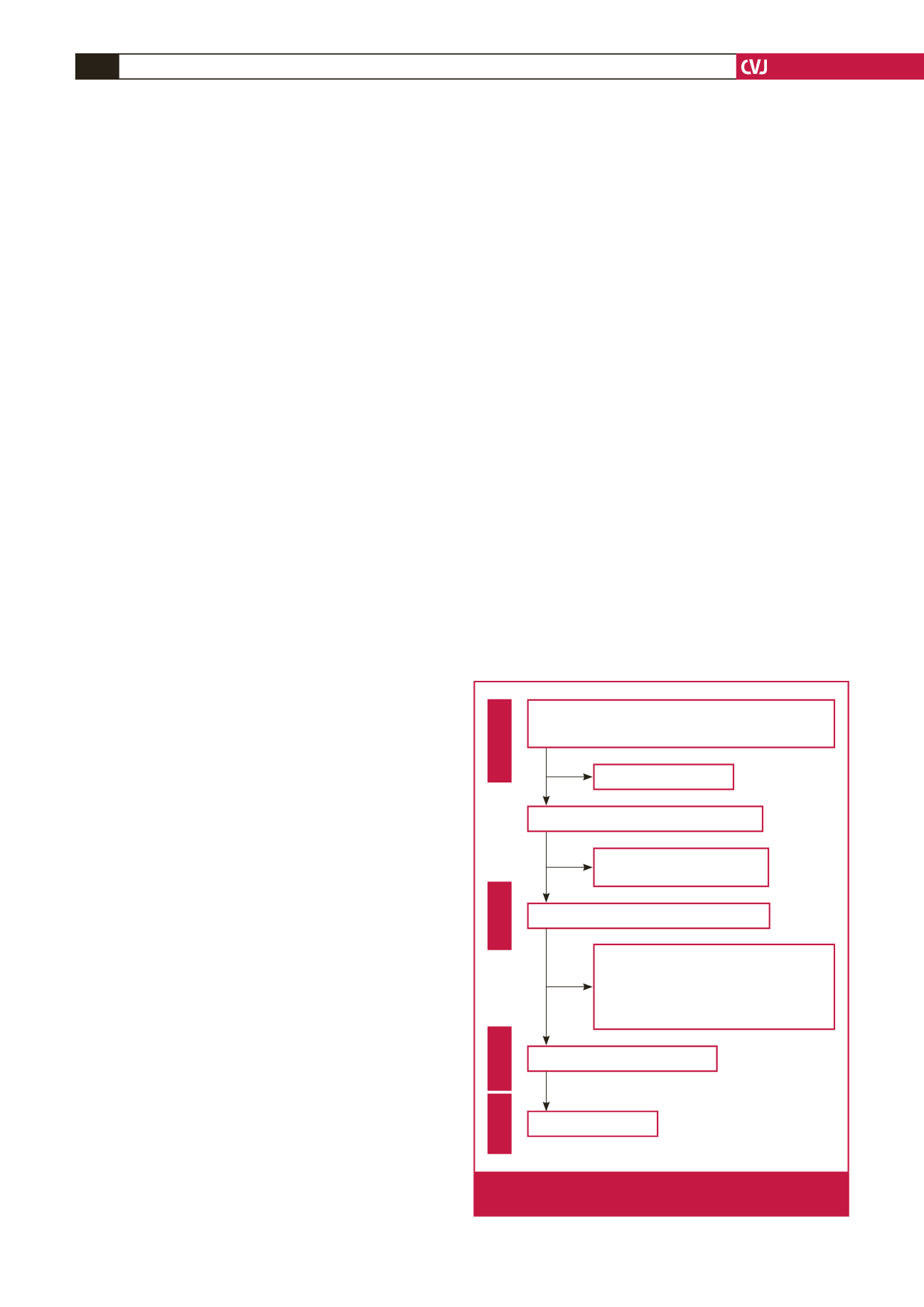
in the PRISMA flow chart (Fig. 1).
Study assessment for inclusion and exclusion criteria and
data extraction were conducted by two independent assessors
(AO and APO) based on the descriptions in the original
article. Only studies with usable data and appropriate analytical
techniques were included in the meta-analysis. The following
information was extracted from each included study: first author
name, publication year, sample size, average follow-up time, the
incidence of CVD, adjusted relative risk (RR)/hazard ratio and
95% confidence interval (CI), etc.
Studies included in this meta-analysis were prospective cohort
reports (where the primary exposure was GLV consumption and
outcomes were CVD events) only. Where there are significant
levels of data overlap among published studies, the study with
complete evidence was included in the quantitative synthesis.
A methodological assessment for risk of bias of included
studies was conducted (independently by two members of the
review team) using the Newcastle–Ottawa scale for quality
assessment of observational reports
36
following the Cochrane
Collaboration guidelines.
37
Statistical analysis
Using the RR and 95% CI for highest quintile/category of GLV
consumption compared to the lowest quintile/category of GLV
Records retrieved via electronic catalogue search
Google Scholar, EMBASE, MEDLINE, HINARI and
Cochrane Library (
n
= 3 132)
Full-text articles appraised for eligibility (
n
= 85)
Identification
68 full-text articles exempted, with reasons:
• 29 without data on GLV
• 18 animal and
in vitro
studies
• 14 reviews, abstract, letters and case report
• 6 cross-sectional reports
• 1 registered trial
Articles eligible for inclusion (
n
= 17)
Prospective studies (17)
Eligibility
Included
Screening
Records after excluding duplicates (
n
= 2 102)
1 030 duplicates excluded
2 017 records excluded after
examining titles and abstracts
Fig. 1.
PRISMA flowchart describing selection of the stud-
ies for the meta-analysis



















