CARDIOVASCULAR JOURNAL OF AFRICA • Vol 22, No 5, September/October 2011
AFRICA
265
people had hypertension and were not receiving antihypertensive
medication. Importantly, when defining global cardiovascular
risk profiles according to the SAHS/ESH/ESC guidelines,
16,27
6.7% of people have untreated hypertension together with a high
or very high added cardiovascular risk. The disturbing cardiovas-
cular risk profiles of untreated hypertensives at a high or very
high added risk were characterised by the presence of severe
hypertension (systolic BP
≥
180 mmHg or diastolic BP
≥
110
mmHg) in ~52%, and the presence of DM in ~33%. In contrast,
no untreated hypertensives with lower risk profiles had either
severe hypertension or DM.
Although a number of studies have reported on the prevalence
of untreated hypertension in a variety of countries,
8-13
including
South Africa,
12,13
the present study extends on these studies by
reporting on the global cardiovascular risk profiles of untreated
hypertensives who are at sufficient risk to consider immediate
antihypertensive therapy. In this regard, based on the SAHS/
ESH/ESC guidelines,
16,27
6.7% of these participants (69 of 1 029
participants with a high or very high added risk) were at an
absolute 10-year risk of cardiovascular disease of 20–30% (high
added risk) or
>
30% (very high added risk).
16
Therefore, over
10 years, a minimum of 1 740 cardiovascular events could occur
per 100 000 of the population of African ancestry living in urban,
developing communities in South Africa through a lack of anti-
hypertensive drug therapy. This clearly represents a considerable
health burden mediated by a lack of drug therapy.
Although in the present study we focused our assessment of
global cardiovascular risk prediction based on the SAHS/ESH/
ESC guidelines,
16,27
we also calculated global cardiovascular risk
from the WHO/ISH risk prediction charts for low- and middle-
income countries.
28
We preferentially focused on the SAHS/
ESH/ESC guidelines for a number of reasons. Importantly,
WHO/ISH risk charts exclude an analysis that incorporates the
risk for obesity. In this regard, we have previously demonstrated
that obesity is highly prevalent and independently contributes
to cardiovascular damage in urban, developing communities in
South Africa.
18-24
Furthermore, WHO/ISH risk charts exclude
an assessment of risk in the 20–40-year age category and we
have noted that a significant burden of severe hypertension (BP
≥
180/110 mmHg) exists in participants younger than 40 years
of age.
In contrast, the SAHS/ESH/ESC guidelines incorporate the
risk of adiposity and allow for an assessment of risk in all age
groups.
16,27
Moreover, the recommendation for drug intervention
using the WHO/ISH charts has been suggested to be a
>
30%
risk of a cardiovascular event in 10 years,
28
which in the popula-
tion we studied, was likely to have excluded a number of severe
hypertensives. Although our focus was on the approach adopted
by the SAHS/ESH/ESC guidelines, global cardiovascular risk
scores identified using the two approaches were similar, there-
fore justifying a focus on one approach alone.
In contrast to the South African Health and Demographic
Survey conducted in 1998, where only 21% of black hyperten-
sives were receiving antihypertensive medication,
12
in the present
study, approximately 51% of hypertensives were receiving
therapy. This clearly represents improved care at a primary-care
level in urban, developing communities in South Africa in this
ethnic group. This ~51% of hypertensives receiving therapy is
a proportion much closer to that obtained in developed nations
such as the USA, where 60.4% are receiving treatment,
8
and also
much closer to the proportion of white hypertensives receiving
treatment in South Africa in 1998 (~55%).
12
However, as pointed out in the aforementioned discussion,
the caveat to this improved antihypertensive care, compared
to previous studies,
12
is that 6.7% of the remaining untreated
hypertensives were at a sufficiently high risk of a cardiovascular
event that drug treatment should have been initiated. Moreover,
half of these high-risk untreated hypertensives were at a high
risk because of the presence of severe hypertension, and a third
because of the presence of DM. In contrast, none of the partici-
pants in the lower-risk categories had either severe hypertension
or DM. These data indicate that it is necessary to introduce
programmes at a community level to identify hypertensives with
severe hypertension or DM.
Although not a primary aim of this study, it is nevertheless
important to comment on the control of BP in treated hyperten-
sives. In this regard, only 35.9% of treated hypertensives were
controlled to target BP levels. This is in contrast to the 59.7%
of white hypertensives and 48.9% of black hypertensives that
are controlled to target BP levels in the USA.
8
However, the data
obtained in the present study are in keeping with the 33% of
hypertensive peri-urban black South Africans that achieved BP
control in alternative studies.
14,15
A possible explanation for the low BP control rates in the
treated hypertensives in the present study is therapeutic inertia.
31
Indeed, ~70% of treated hypertensives were receiving mono-
therapy only, and it is presently well accepted that monotherapy
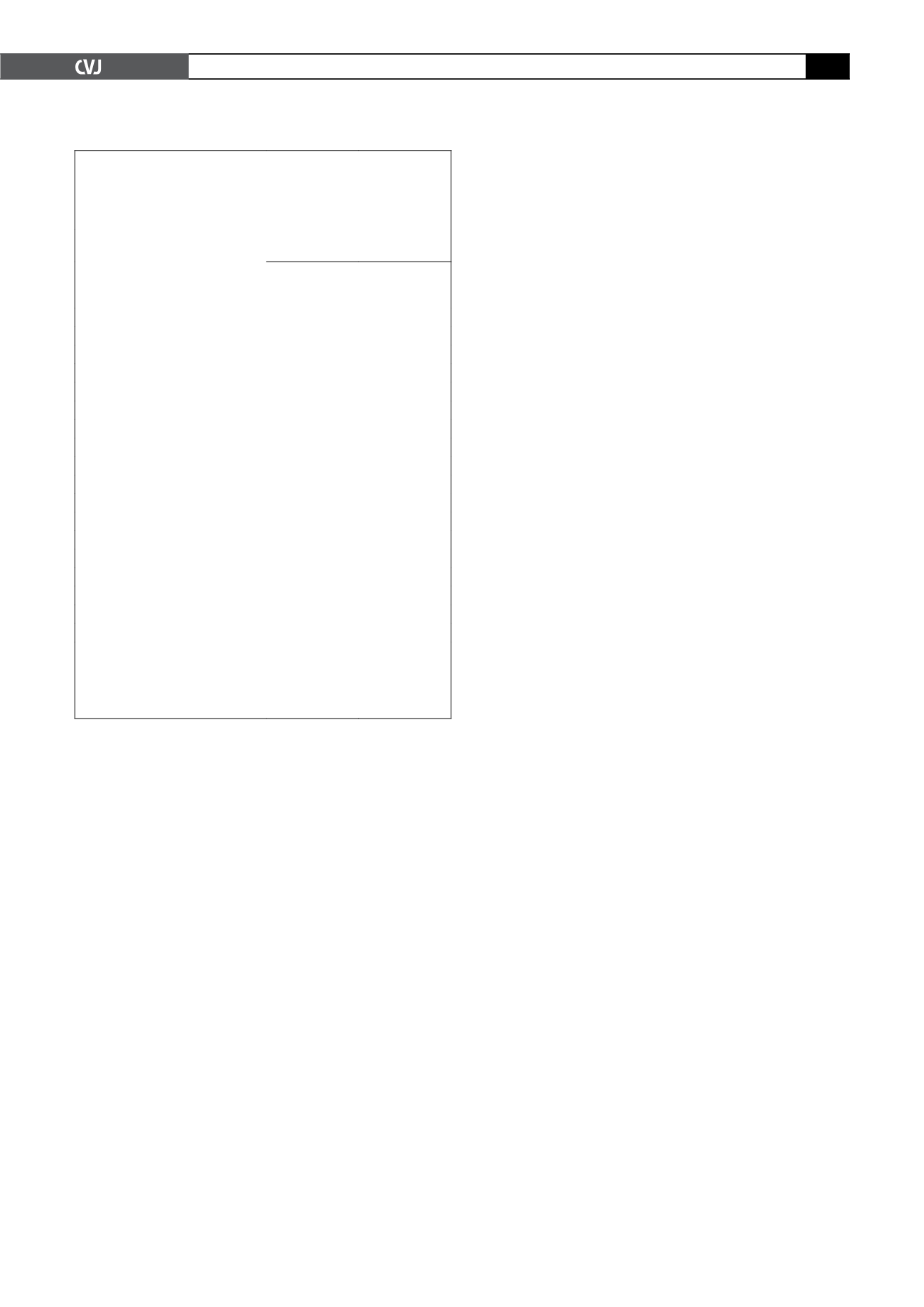
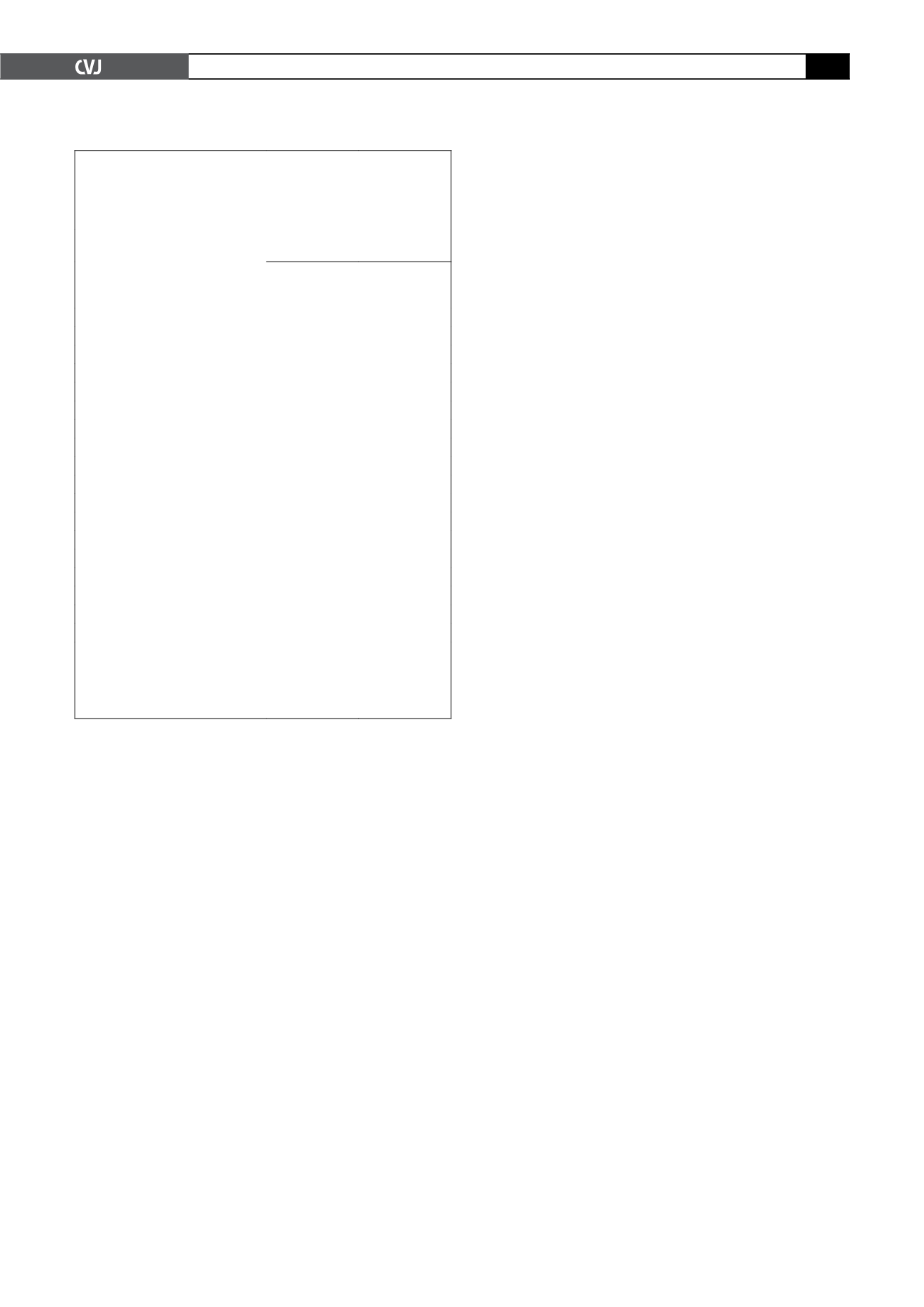
TABLE 4. CHARACTERISTICS OF UNTREATED HYPERTEN-
SIVESWITH DIFFERENT CARDIOVASCULAR RISK CATEGO-
RIES BASED ON THE SOUTHERNAFRICAN HYPERTENSION
SOCIETY,
27
AND EUROPEAN SOCIETY OF HYPERTENSION/
EUROPEAN SOCIETY OF CARDIOLOGY
16
GUIDELINES
Untreated hypertensives with
cardiovascular risk score of:
High or very
high added
Average, low
added, or
moderate added
Number
69
164
Age (years)
59.2
±
14.0*
46.7
±
15.2
% at risk age
45*
18
% female
59.4
53.7
Body mass index (kg/m
2
)
31.3
±
6.4*
30.3
±
7.9
% overweight/obese
26.1/58.0*
23.2/48.2
Waist circumference (cm)
97.0
±
12.9*
92.9
±
16.2
Central obesity (%)
67.7*
43.2
Regular tobacco intake (% subjects)
23.2
20.7
Regular alcohol intake (% subjects)
26.1
28.1
% with diabetes mellitus
33.3**
0
% with dyslipidaemia
33.3*
21.3
% with CVD
8.7*
0
% with elevated serum creatinine
4.4
2.4
Severity of increased BP
% with stage I BP
†
34.8*
67.1
% with stage II BP
†
13.0*
32.9
% with stage III BP
†
52.1**
0
CVD: cardiovascular disease.
†
See text for definitions. High added indi-
cates 20–30% risk of either a myocardial infarct or a stroke over 10 years.
Very high added indicates
>
30% risk of either a myocardial infarct or a
stroke over 10 years, *
p
<
0.0001 vs other group. Bold values indicate
significant differences between the groups.