CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 4, May 2012
AFRICA
209
distension of the inferior vena cava that does not diminish with
inspiration, which is a manifestation of the elevated venous
pressure in tamponade.
6
In addition, there can be marked
reciprocal respiratory variation in mitral and tricuspid flow
velocities. Tricuspid flow increases and mitral flow decreases
during inspiration (the reverse in expiration).
Achallengingdifferentialdiagnosisisendomyocardialfibrosis,
a common form of restrictive cardiomyopathy (RCM) in Africa.
7
Because constrictive pericarditis can be corrected surgically, it
is important to distinguish chronic constrictive pericarditis from
restrictive cardiomyopathy, which has a similar physiological
abnormality, i.e. restriction of ventricular filling. Helpful in
the differentiation of these two conditions are right ventricular
trans-venous endomyocardial biopsy (by revealing myocardial
infiltration or fibrosis in RCM) and echocardiography, CT
scan or cardiac magnetic resonance imaging (by demonstrating
a thickened pericardium in constrictive pericarditis but not
in RCM).
8
Our fourth patient (MN) actually presented this
challenge but a convincing thickening of the pericardium at
echocardiography was enough to help us clarify the diagnosis.
Another important problem is the lack of placebo-controlled
trials from which appropriate therapy may be selected, and
of guidelines that assist in important clinical decisions. As a
result, the practitioner must rely heavily on clinical judgment.
9
The absence of guidelines specific to this subset of pericardial
disease may be due to its relative rarity in the Western world.
The recent European Society of Cardiology guidelines on
management of pericardial diseases was also silent on the subset
of patients with effusive constrictive pericarditis, presumably
due to a paucity of data on the subject.
6
Other reasons could be
difficulty in reaching a diagnosis and varied aetiopathogenesis,
necessitating different evolution patterns.
While there is an abundance of diagnostic armamentarium
in the West, practitioners in sub-Saharan Africa largely have to
cope with severe limitations in diagnostic facilities. An exception
to this may be South Africa, where a recent report highlighted
the value of contrast-enhanced magnetic resonance imaging
(MRI) in delineating epicardial and pericardial inflammation in
effusive–constrictive pericarditis.
10
Cost is still an issue even if
MRI becomes widely available. Clinical acumen and reasoning
therefore still form the bedrock of clinical practice in most
centres.
The cases managed in this series illustrate this point. In only
two of the five cases was there a hint of constrictive physiology
at the initial echocardiography, even though it is known there is
a phase of transient sub-acute constriction, which may improve
after pericardial drainage and medical treatment, especially
with anti-tuberculous therapy in those arising secondary to
tuberculosis. The only strong evidence of a high likelihood of
need for pericardiectomy was the duration of the history in the
first three patients. They all had a history longer than two years,
suggestive of a chronic process.
Reaching an aetiological diagnosis is a real challenge globally
but more problematic in our local practices. The results of
pericardial fluid culture are frequently falsely negative and
pericardial biopsy has a higher yield of diagnostic specimens.
11-13
One therefore has to rely on pericardial tissue biopsymicrobiology
and histology. None of our patients had positive evidence from
pericardial fluid microbiology or cytology. The histology of
their pericardia is shown in Table 1. Three of the patients were
therefore treated empirically with anti-tuberculous therapy.
The difficulty in establishing a bacteriological or histological
diagnosis is foremost among unresolved issues in patients
with pericarditis.
14
A definite or proven diagnosis is based on
demonstration of tubercle bacilli in the pericardial fluid or on
histological section of the pericardium. A probable or presumed
diagnosis is based on proof of tuberculosis elsewhere in a
patient with otherwise unexplained pericarditis, a lymphocytic
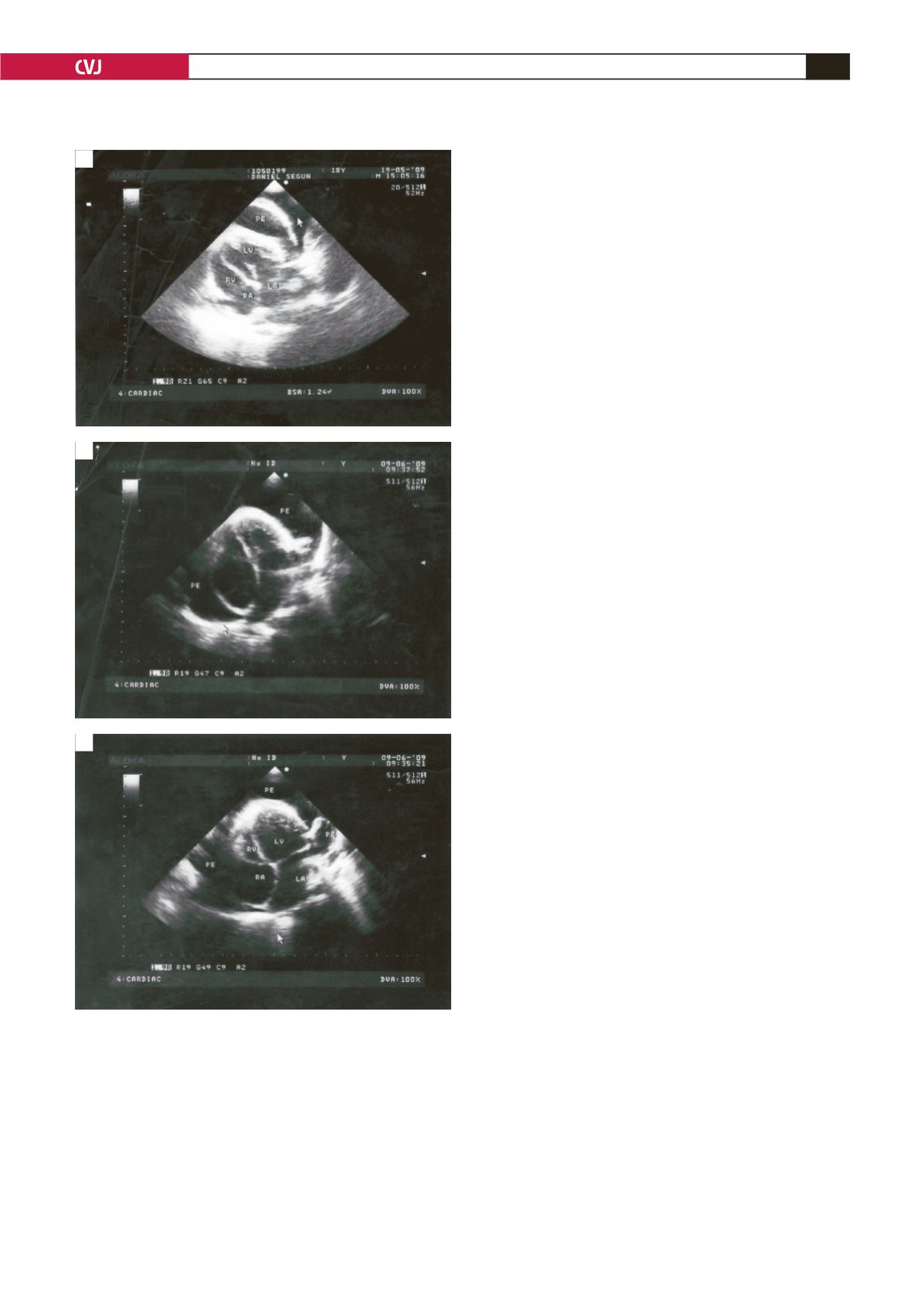
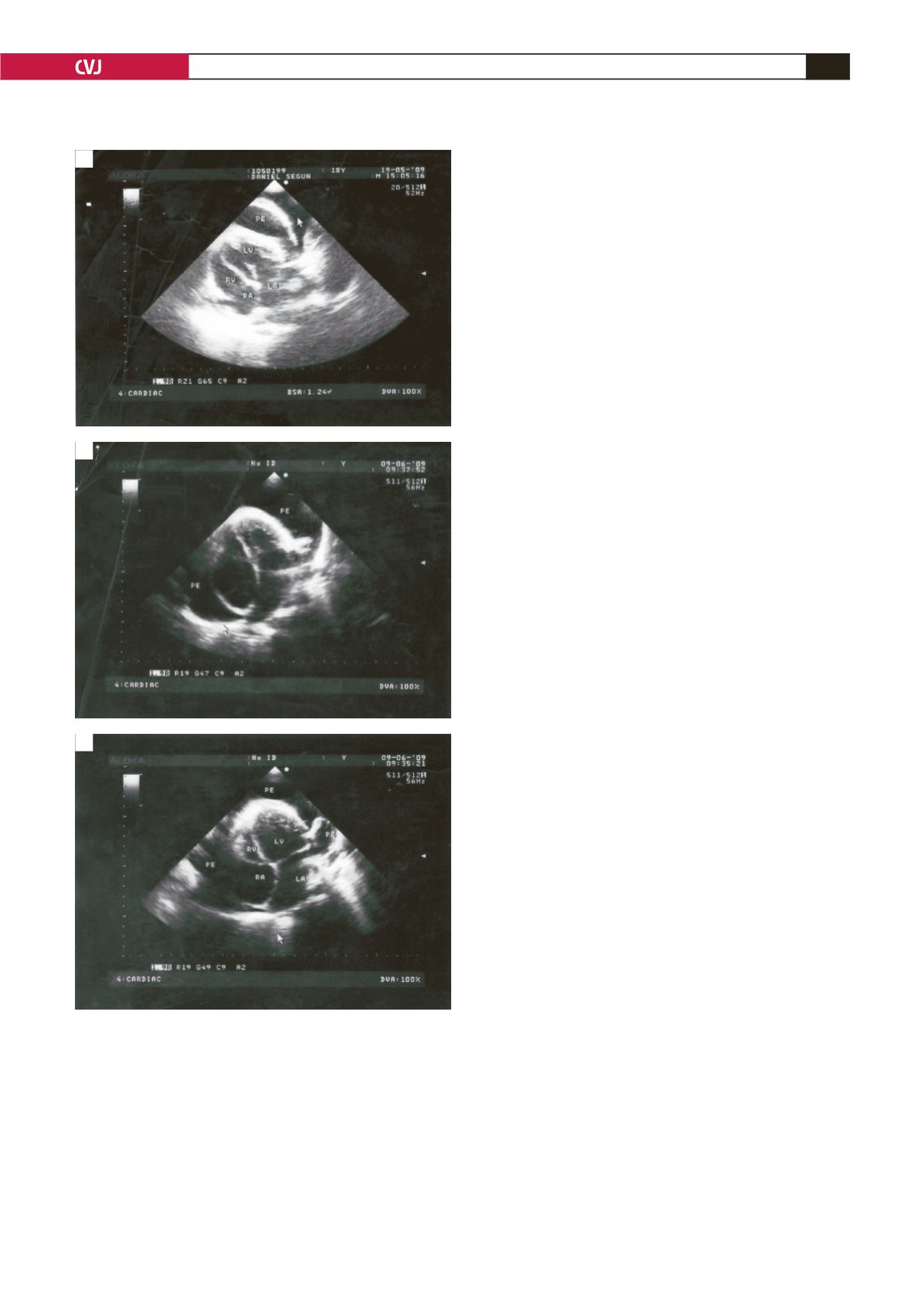
Fig. 4. Echocardiography showing moderate pericardial
effusion (PE). RV = right ventricle; LV = left ventricle; RA
= right atrium; LA = left atrium.
A
B
C