CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 5, June 2012
296
AFRICA
in combination with the use of digoxin.
I would imagine that there will be a
significant increase in the use of
eplerenone with the perceived benefit of
a better side-effect profile.
A new indication for the sinus node
inhibitor ivabradine
This agent will enjoy much wider use in
a substantial number of patients, given
the qualifying criteria for use. I would
hope that the pricing will improve with
increase in the number of prescriptions.
An expanded indication for cardiac
resynchronisation therapy (CRT)
With the proper selection of patients,
there is still a significant proportion of
patients who qualify for CRT. The cost
implication is a given, but in the long
run, this is cost saving in comparison to
the cost of repeated hospitalisations and
indirect cost of death.
New information on the role of
coronary revascularisation in systolic
heart failure
The changing epidemics in coronary
artery disease risk factors, especially in the
developing world, will mean an increase
in invasive interventions in the heart
failure population as well. Infrastructural
and human resource development are also
imperative for the standard of care to be
adequate in the not-so-distant future.
Recognition of the growing use of
ventricular assist devices (VADs)
This is idealistic and will still not be a
widely available treatment avenue. This is
of course of major importance where the
indication for appropriate use is met. The
cost implication as well as availability
remain deterrents for most nations.
The emergence of transcatheter valve
interventions
This is a further reflection of the evolution
in the practice of medicine and cardiology
in particular. I find these exciting but
the economic realities dampen one’s
enthusiasm. There may be a balance in
the future as these interventions become
more widely used and readily available.
Julia Aalbers
1.
ESC guidelines for the diagnosis and treat-
ment of acute and chronic heart failure
2012.
Eur Heart J
. Doi 10.1093/eurheartj/
ehs104..
2.
ESC Press Conference, Belgrade, 20 May
2012.
3.
Boom NK, Lee DS, Tu JV. Comparison of
processes of care and clinical outcomes for
patients newly hospitalised for heart failure
attended by different physician specialists.
Am Heart J
2012;
163
: 252–259.
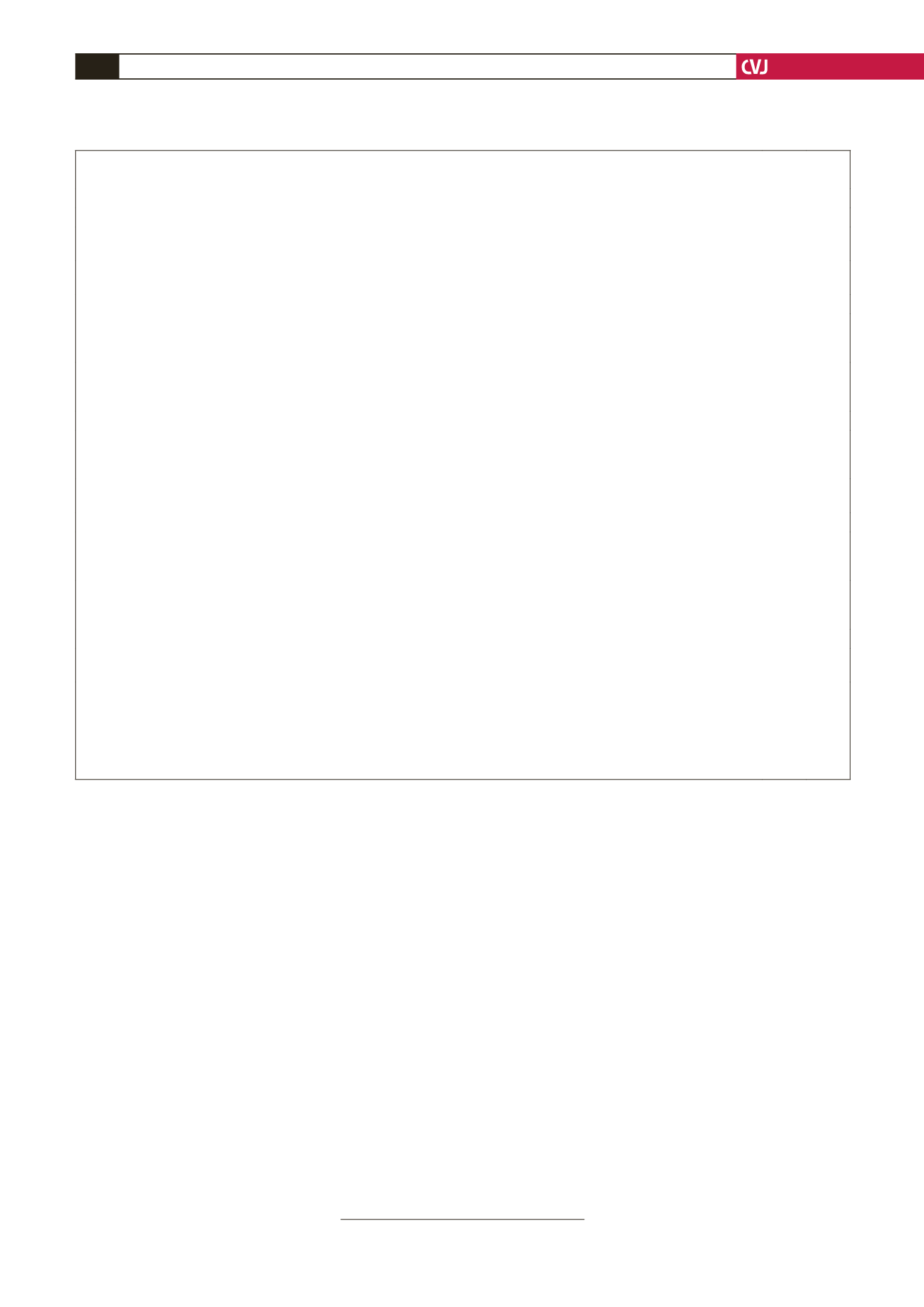
TABLE 2. OTHER TREATMENTSWITH LESS CERTAIN BENEFITS IN PATIENTSWITH SYMPTOMATIC
(NYHA CLASS II–IV) SYSTOLIC HEART FAILURE
Recommendations
Class
a
Level
b
ARB
Recommended to reduce the risk of heart failure hospitalisation and the risk of premature death in patients with an EF
≤
40% and
unable to tolerate an ACE inhibitor because of cough (patients should also receive a beta-blocker and an MRA).
I
A
Recommended to reduce the risk of heart failure hospitalisation in patients with an EF
≤
40% and persisting symptoms (NYHA
class II–IV), who are unable to tolerate an MRA, despite treatment with an ACE inhibitor and a beta-blocker.
c
I
A
Ivabradine
Should be considered to reduce the risk of heart failure hospitalisation in patients in sinus rhythm with an EF
≤
35%, a heart rate
remaining
≥
70 beats/min, and persisting symptoms (NYHA class II–IV) despite treatment with an evidence-based dose of beta-
blocker (or maximum tolerated dose below that), ACE inhibitor (or ARB), and an MRA (or ARB).
d
IIa
B
May be considered to reduce the risk of heart failure hospitalisation in patients in sinus rhythm with an EF
≤
35% and a heart rate
≥
70 beats/min who are unable to tolerate a beta-blocker. Patients should also receive an ACE inhibitor (or ARB) and an MRA
(or ARB).
d
IIb C
Digoxin
May be considered to reduce the risk of heart failure hospitalisation in patients in sinus rhythm with an EF
≤
45% who are unable
to tolerate a beta-blocker (ivabradine is an alternative in patients with a heart rate
≥
70 beats/min). Patients should also receive an
ACE inhibitor (or ARB) and an MRA (or ARB).
IIb B
May be considered to reduce the risk of heart failure hospitalisation in patients with an EF
≤
45% and persisting symptoms
(NYHA class II–IV) despite treatment with a beta-blocker, ACE inhibitor (or ARB), and an MRA (or ARB).
IIb B
H-ISDN
May be considered as an alternative to an ACE inhibitor or ARB, if neither is tolerated, to reduce the risk of heart failure
hospitalisation and risk of premature death in patients with an EF
≤
45% and dilated LV (or EF
≤
35%). Patients should also
receive a beta-blocker and an MRA.
IIb B
May be considered to reduce the risk of heart failure hospitalisation and risk of premature death in patients in patients with an EF
≤
45% and dilated LV (or EF
≤
35%) and persisting symptoms (NYHA class II–IV) despite treatment with a beta-blocker, ACE
inhibitor (or ARB), and an MRA (or ARB).
IIb B
PUFAs
An n-3 PUFA
e
preparation may be considered to reduce the risk of death and the risk of cardiovascular hospitalisation in patients
treated with an ACE inhibitor (or ARB), beta-blocker and an MRA (or ARB).
IIb B
ACE
=
angiotensin converting enzyme; ARB
=
angiotensin receptor blocker; CHARM-Added
=
Candesartan in Heart Failure: Assessment of
Reduction in Mortality and Morbidity-Added; EF
=
ejection fraction; H-ISDN
=
hydralazine and isosorbide dinitrate; MRA
=
mineralocorticoid
receptor antagonist; NYHA
=
NewYork Heart Association; PUFA
=
polyunsaturated fatty acid.
a
Class of recommendation;
b
Level of evidence;
C
In the CHARM-Added trial, candesartan also reduced cardiovascular mortality;
d
European Medecines Agency has approved ivabradine for use in patients with a heart rate
≥
70 beats/min;
e
Preparation studied in cited trial; the GISSI-HF trial had no EF limit.