CARDIOVASCULAR JOURNAL OF AFRICA • Vol 23, No 5, June 2012
e2
AFRICA
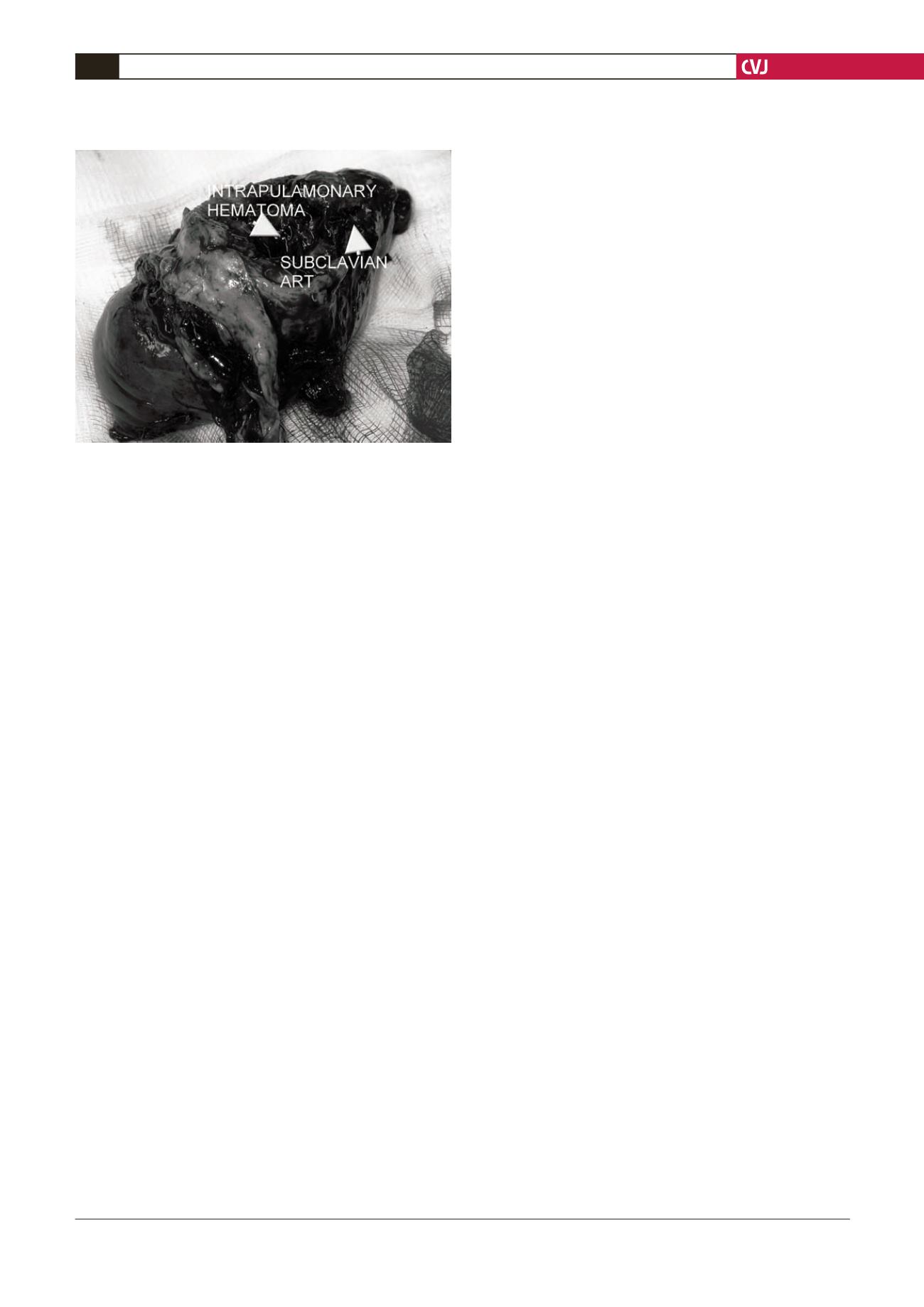
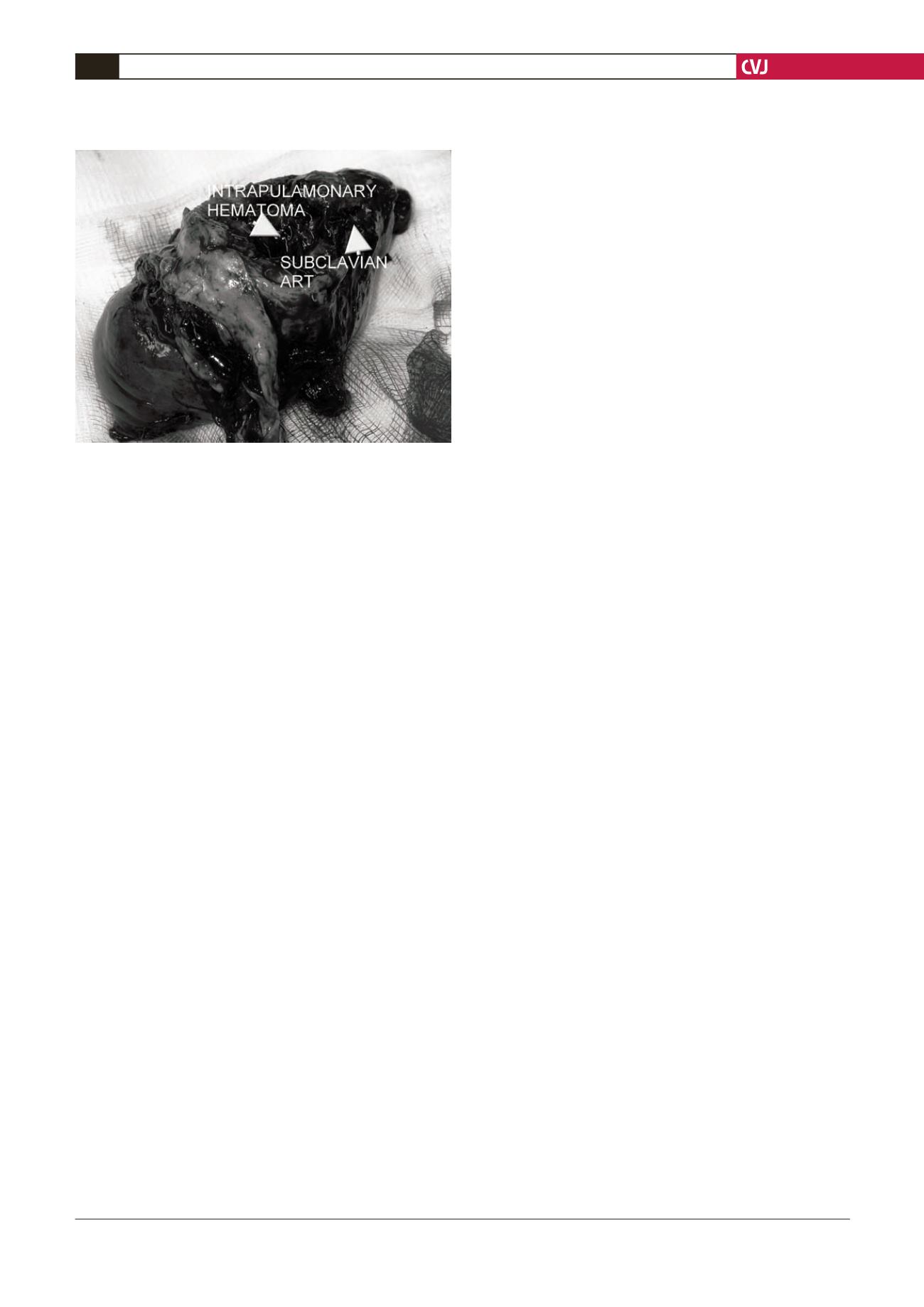
Macroscopically the surgical specimen showed the ruptured
subclavian artery running into the left lung apex and associated
with a giant pulmonary haematoma (Fig 3). The continuity of
the subclavian artery was restored with a reversed saphenous
vein graft, which was harvested before the thoracotomy. The
blood loss was estimated to be approximately 350 cm
3
. The
postoperative course was uneventful and the patient was
discharged on the 10th postoperative day.
Discussion
An infected artery may rupture in the absence of aneurysmal
dilatation.
7
The pathogenesis, however, remains unclear in
many cases. The commonest site of endarterial infection is the
abdominal aorta.
8
Infection of the main intrathoracic arteries
is rarely reported and may present as haemoptysis,
3
or it may
mimic a bronchogenic carcinoma.
4
In our case, the infected site
had been used as an injection site. The infection caused the
vascular wall to erode into the left lung and the intrapulmonary
artery to rupture.
Early diagnosis is important because untreated mycotic
subclavian arterial disease has a dismal outcome. Therefore a high
index of suspicion must be maintained. Moreover, haemoptysis
due to subclavian arteritis has not been documented before.
Numerous organisms can cause infection in the arterial wall but
the most frequent is
Salmonella
, which is found in 36% of cases.
It has a predilection for larger, diseased blood vessels. Other
organisms known to cause such infection are staphylococci,
streptococci,
Escherichia coli, Pseudomonas, Bacteroides,
Haemophilus, Clostridia
and
Enterobacter klebsiella
.
Predisposing factors to infective endarteritis include pre-existing
atherosclerosis, aneurysms, diabetes, immunosuppression or
active vasculitis.
An early diagnosis allows both prompt, appropriate antibiotic
treatment and timely surgical intervention before invasive
pathogens destroy the arterial wall. Early diagnosis may be aided
by greater awareness and improved radiological techniques such
as ultrasonography, computer-aided tomography and digital
subtraction angiography. In particular, enhanced computed
tomography may demonstrate changes in the size or appearance
of the infected artery or show peri-arterial nodularity, air or pus
in the arterial wall. Arteriography is not specific but may show
atheromatous disease or a saccular or multiloculated aneurysm in
an otherwise normal vessel, suggesting a local infection.
6
The accepted management of bacterial arteritis is intravenous
antibiotic therapy, excision and debridement of the artery and
the mycotic false aneurysm if present, and where possible, extra-
anatomical vascular reconstruction along an uncontaminated
path. Surgical treatment for patients with subclavian arteritis
should be considered in cases of unremitting infection after
adequate antibiotic treatment, or rupture, and to avoid embolus
formation or thrombosis. In our case, emergency surgical
management was indicated because the recurrent severe
haemoptysis had to be controlled.
A variety of techniques are used with different surgical
approaches and arterial repair. Surgical approaches include supra-
clavicular incision, axillary incision, median sternotomy with a
transverse incision along the second rib bed, and posterolateral
thoracotomy, or a combination of all of these, depending on the
location of the aneurysm.
Conclusion
In our case, a left posterolateral thoracotomy was performed
through the fourth intercostal space with the patient under
anaesthesia, using double-lumen endotracheal intubation.
It provided a good approach to perform the excision and
reconstruction of the subclavian artery and to perform a
concomitant left upper lobectomy. A reversed saphenous vein
bypass graft was used to reduce the risk of secondary blood-borne
infection, which is associated with using prosthetic materials.
9
References
1.
Saliou C, Badia P, Duteille F, D’Attellis N, Ricco JB, Barbier J.
Mycotic aneurysm of the left subclavian artery presented with hemop-
tysis in an immunosuppressed man: case report and review of literature.
J Vasc Surg
1995;
21
(4): 697–702.
2.
Iijima K, Kuribayashi R, Sakarada T, Sekine S, Aida H, Abe T. [A left
subclavian arterial aneurysm ruptured into the left lung – a case report].
Nippon Kyobu Geka Gakkai Zasshi
1992;
40
(3): 440–443.
3.
Takagi H, Mori Y, Umeda Y, Fukumoto Y, Yoshida K, Shimokawa K,
Hirose H. Proximal left subclavian artery aneurysm presenting hemop-
tysis, hoarseness, and diplopia: repair through partial cardiopulmonary
bypass and perfusion of the left common carotid artery.
Ann Vasc Surg
2003;
17
(4): 461–463.
4.
Boundy K, Bignold LP. Syphilitic aneurysm of the right subcla-
vian artery presenting with hemoptysis.
Aust NZ J Med
1987;
17
(5):
533–535.
5.
Deulofeu Fontanillas F, Barbeta Sánchez E, Bernet Vidal M, Sentis
Criville M, Pujol Farriols R. [Massive hemoptysis secondary to
mycotic aortic aneurysm].
Ann Med Interna
1989;
6
(7): 373–375.
6.
Wu MH, Lai WW, Lin MY, Chou NS. Massive hemoptysis caused by
a ruptured subclavian artery aneurysm.
Chest
1993;
104
(2): 612–613.
7.
Mii S, Ienaga S, Motohiro A, Okadome K. An unusual symptom of
subclavian artery aneurysm: hemoptysis.
J Vasc Surg
1991;
14
(2):
243–245.
8.
Oz MC, Brener BJ, Budas JA,
et al
. A ten-year experience with bacte-
rial aortitis.
J Vasc Surg
1989;
10
: 439–449.
9.
Visrutaratna P, Charoenkwan P, Saeteng S. Mycotic aneurysm of the
left subclavian artery: CT findings.
Singapore Med J
2006;
47
(1):
77–79.
Fig. 3. The surgical specimen showing the ruptured
subclavian artery and left lung apex associated with a
giant pulmonary haematoma.