CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 8, September 2013
314
AFRICA
included pain, itching, limb heaviness, cramps, restless leg and
distress about cosmetic appearance. CEAP (Clinical, aEtiology,
Anatomical and Pathology) class was determined. All the
patients’ height and body weights were measured. The body
mass index was verified with the following formula: weight (kg)/
height
2
(m).
13
In all patients, the potential risks and benefits of endovenous
radiofrequency ablation therapy were explained, and written
informed consent was obtained. Additionally, throughout the
study the principles of the Helsinki Declaration were strictly
followed.
Doppler venous scanning was performed on all patients in
order to document the extent and severity of the reflux in the
great saphenous vein and to evaluate the deep venous system.
Doppler imaging of the patients was performed by Aloka
Prosound Alpha 7 (Hitachi Aloka Medical, Japan) using 5- and
7-mHz linear probes.
Reflux was determined at the saphenofemoral and
saphenopoliteal junctions in the standing position using the
Valsalva manoeuvre or manual distal compression with rapid
release. Pathological venous reflux was defined as a reverse flow
extending for 0.5 seconds or longer. The localisation and severity
of the venous reflux and sonographic distribution of the varicose
veins were recorded.
Other parameters measured using grey-scale ultrasound in the
standing position are as follows:
•
the diameter of the GSV in the SFJ
•
the diameter of the GSV above the knee
•
the distance of the GSV from the skin above the knee
•
the distance of the GSV from the skin in the middle of the
thigh
•
the length of the GSV that was to be ablated.
Only patients with documented GSV reflux with Doppler
ultrasonography and in CEAP class 2 or above were recruited
into the study. Patients were excluded if there was a significant
reflux in the deep venous system, small saphenous vein or
perforators. Other exclusion criteria included: deep-vein
thrombosis, superficial thrombophlebitis, peripheral arterial
vascular disease, immobility, pregnant or breast-feeding patients,
and previous history of allergy to local anaesthesia.
All cases in this study were performed under general
anaesthesia using a laryngeal mask combined with either
tumescent anaesthesia or a local hypothermia and compression
technique. Electrocardiogram, arterial pressure and oxygen
saturation of the patients were continously monitored. Induction
was achieved with midazolam (0.03 mg/kg), lidocain (1 mg/kg)
and propofol (2 mg/kg). Anaesthesia was maintained with 2%
sevoflurane.
Between January and December 2012 we treated 344 patients
in CEAP clinical class 2–6 with endovenous radiofrequency
ablation. These patients were divided into two groups according
to the anaesthetic management as follows. Group 1: 58 males,
114 females (
n
=
172). Tumescent anaesthesia was given
before the ablation procedure. Group 2: 42 males, 130 females
(
n
=
172). The procedure was performed without tumescent
anaesthesia. Local hypothermia and compression technique was
used.
Patients were placed in the supine position. Prior to
performing RFA, Doppler ultrasonography was used to confirm
the important parameters, including imaging of the GSV and
SFJ, perforators, tributaries, and diameter and treatment length,
to devise an effective operative plan.
A linear 5- or 7-MHz probe was inserted into a sterile cover
and using ultrasound guidance, the GSV was cannulated below
or just above the knee. Following the introduction of a 0.025-
inch guidewire into the GSV, a 4- or 5-Fr intraducer sheath was
advanced over it. The RFA catheter (ClosureFast radiofrequency
ablation catheter, NYSE:COV) was then placed through the
sheath, the guidewire was removed and the tip of the catheter
was placed 2–3 cm distal to the SFJ, just below the superficial
epigastric vein, under ultrasound guidance.
Once proper positioning was confirmed with ultrasound,
a tumescent anaesthetic solution was instilled percutaneously
below the saphenous fascia to surround the vein in group
1 patients. This solution consisted of 500 ml saline, 20 ml
2% prilocaine, 20 ml 8.4% sodium bicarbonate and 0.5 ml
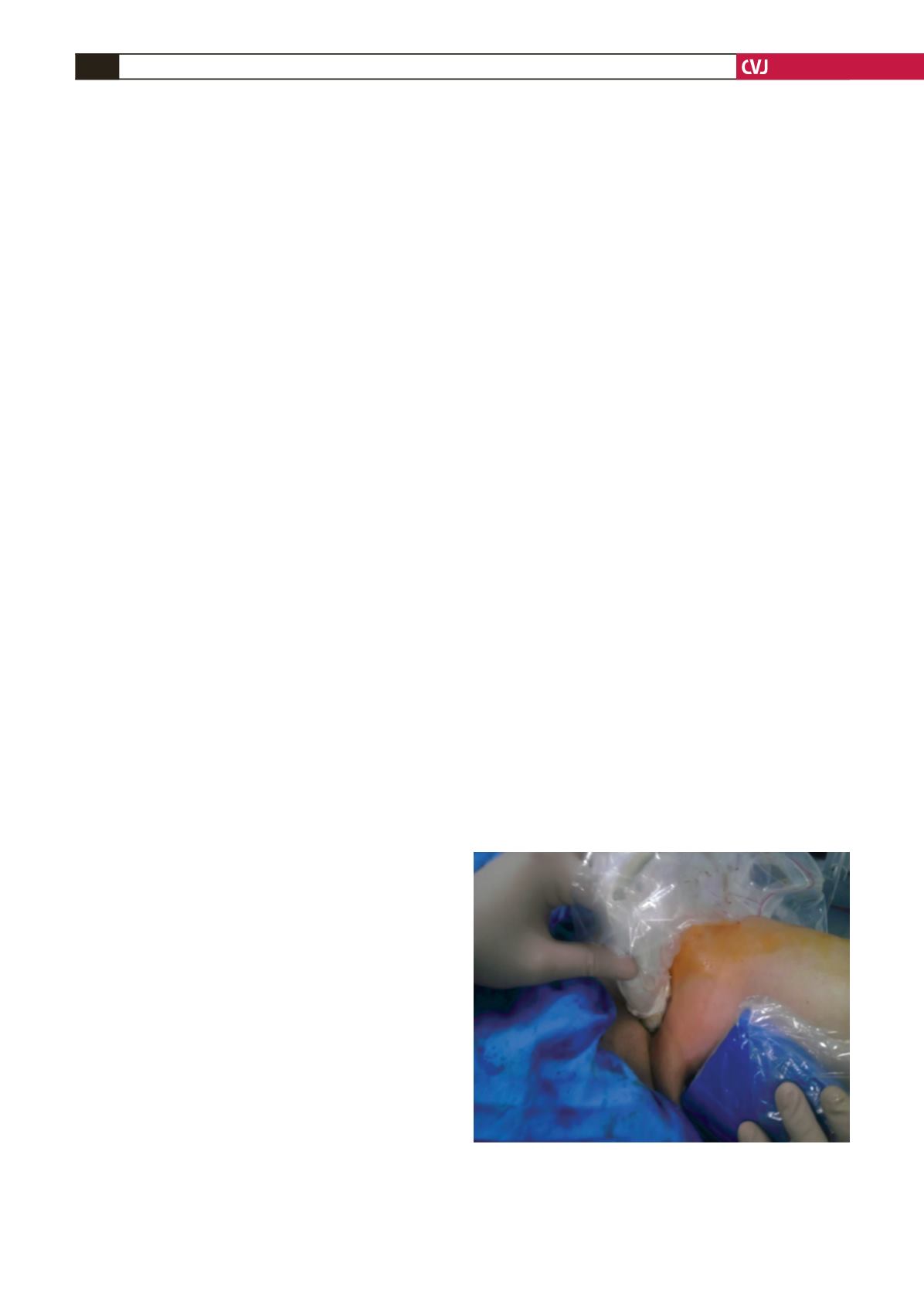
epinephrine. In group 2, instead of local tumescent anaesthesia,
we used a local hypothermia technique (external compression
with ice and dampening the skin with saline (+4°C) in order to
prevent skin burn) (Fig. 1).
The RF generator (VNUS Medical Technologies) was then
activated and delivery of radiofrequency energy was maintained
at 120°C. Radiofrequency ablation was performed at a rate of
40 W per 7 cm. During the procedure, in both groups, sufficient
pressure was exerted with the ultrasound probe to occlude the
SFJ and CFV. Following completion of the procedure, closure
of the GSV and patency of the common femoral vein and
superficial epigastric vein was checked with Doppler ultrasound.
As the last step of the treatment, all varicose veins were removed
by phlebectomy in both groups (Figs 2, 3).
A compression bandage was wrapped around the treated
limb and the patient was encouraged to walk immediately. This
remained in place for three hours. The patients wore class II
(30–40 mmHg) thigh-high compression stocking continously for
the next 24 hours. They then wore the compression stocking only
during the day for the next 15 days. The patients were prescribed
a non-steroidal anti-inflammatory drug, an antibiotic and a veno-
active drug during the postoperative period.
Fig. 1. Local hypothermia and compression technique:
external compression with Doppler probe for preventing
extension of the thrombus to the deep venous system,
and external compression with ice and dampening of the
skin with saline (+4°C) in order to prevent skin burn.