CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 8, September 2013
AFRICA
319
ECG evidence of right ventricular strain was noted in 12% of
deformities. Echocardiography showed mitral valve prolapse in
7.3% of the patients.
The Rawitch repair operative technique was used for all 77
patients. General anaesthesia was given and a Foley catheter
was placed in all patients. Intravenous cefazolin (1 g) was
administered pre-operatively.
A mid-sternal incision was made, and short skin flaps were
elevated superiorly and inferiorly using electrocautery. The
pectoralis major muscle on each side was then reflected laterally
to expose all costal cartilages. The lower costal cartilages are
often covered by the rectus muscles.
The deformed costal cartilages were bilaterally resected
sub-perichondrially for the full length of the deformed segments.
After removal of the costal cartilages, the xiphosternal joint was
transacted to enable a finger to pass below the sternum through
the mediastinum.
When the pleural space was opened, a small chest tube was
inserted for drainage. A transverse wedge osteotomy was made
across the anterior sternum where the sternum angled down to the
depressed posterior region. The sternum of the posterior region
was fractured at the wedge osteotomy without detachment.
Prepared bone or costal cartilage was used to fix the
deformity. It was placed in the osteotomy and secured by two
transferral monofilament, non-absorbable sutures, and in some
cases, a 5-mm stainless steel wire. The perichondrial sheaths
were sutured together over the sternal and costal cartilage repair;
this is termed plication.
Haemostasis was achieved with cautery after a haemovac drain
had been placed between the muscle layer and the cartilaginous
repair. The skin was closed with absorbable subcuticular sutures.
For three patients with very extensive resection of the costal
cartilage, we used stainless steel bars to support the sternum and
prevent flail chest, instead of the standard Kirschner wires (Fig.
4). This method provided excellent mechanical stabilisation of
the chest.
In all 77 patients, the endotracheal tube was removed in
the operating room. The chest tube and haemovac drain were
routinely removed within 48 hours. Intravenous analgesics were
giving for the first three postoperative days and then no narcotic
medications thereafter. Intravenous cefazolin was given for five
additional days. Three patients’ sternal support bar was removed
six months later under general anaesthesia.
Results
A total of 77 patients underwent repair of PE and PC deformities.
Their ages ranged from 10 to 22 years (mean 17 years) (Table
1). The mean duration of the operation was 2.5 hours. Mean
hospitalisation time was seven days and all patients returned to
work or school about 15 days after the operation.
Before the operation, the most frequent symptoms were
aesthetic and cosmetic. Physiological disorders were present
in 52%, and other symptoms, which were present to varying
degrees, were common: dyspnoea occurred in 20%, and a
compression type of discomfort in the lower anterior chest or
chest pain occurred in 15%. Palpitations and/or tachycardia were
experienced by 8%. Exercise-induced wheezing was reported in
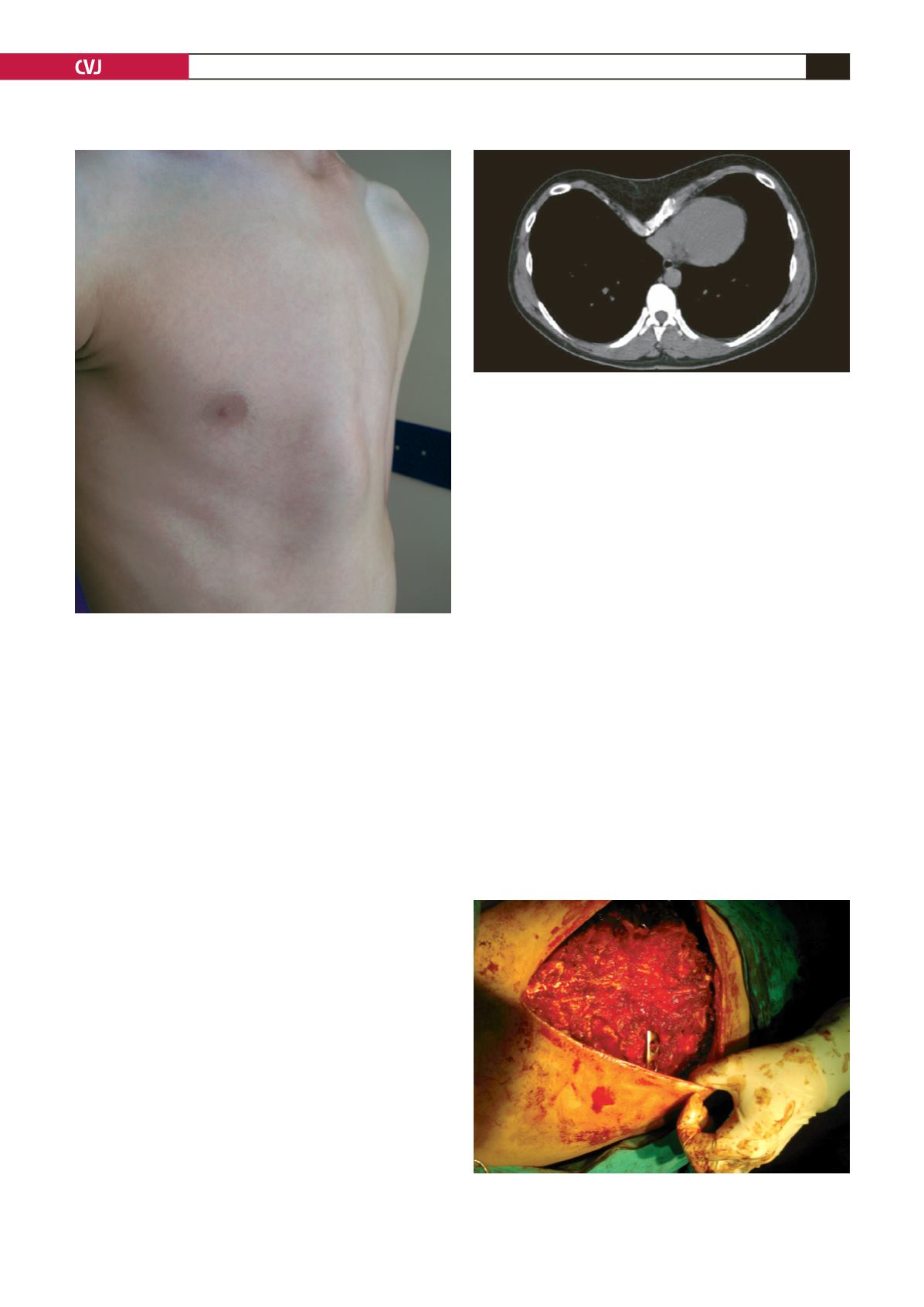
Fig. 2. A patient with pectus carinatum.
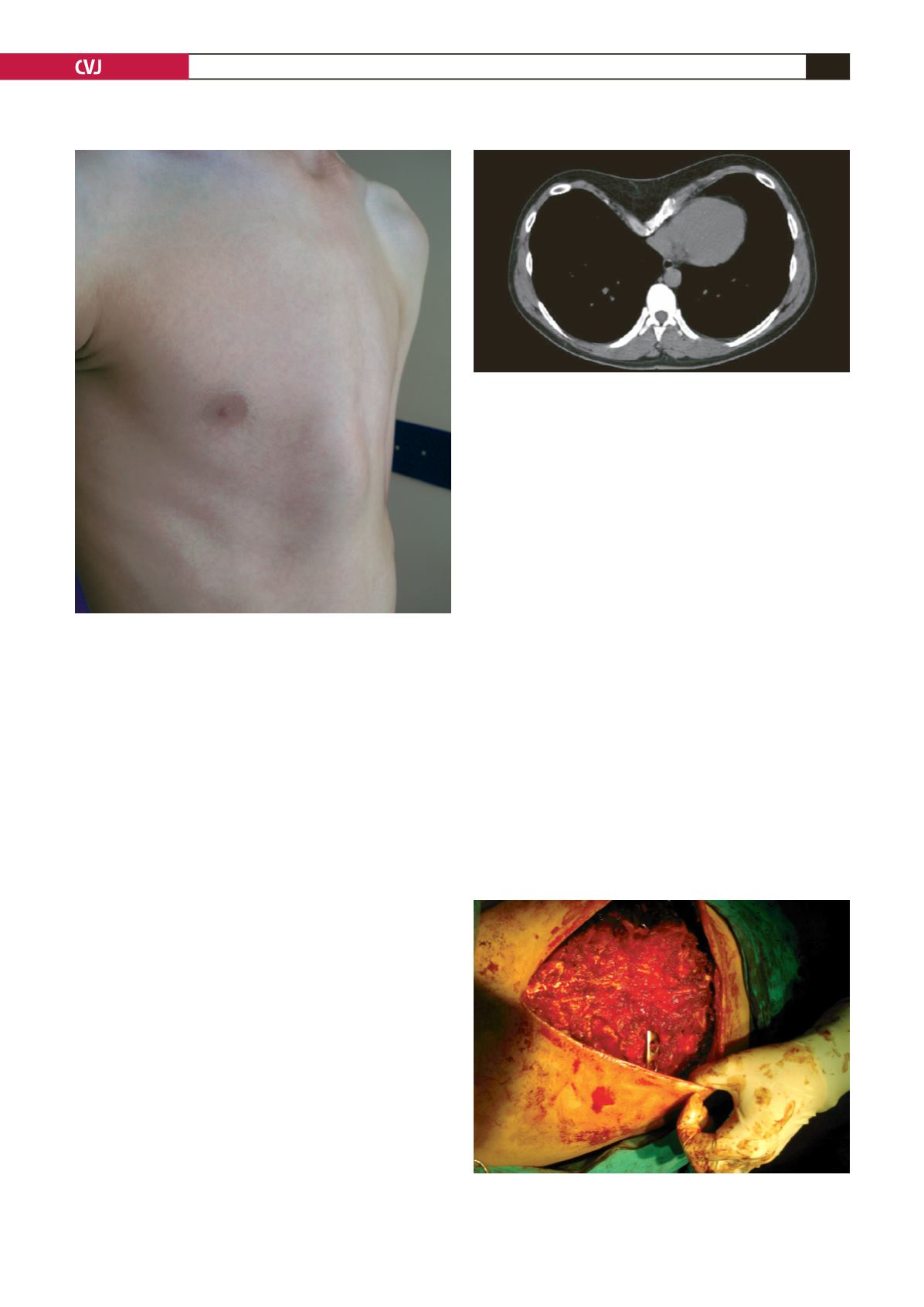
Fig. 3. Computed tomography of the chest showing the
severity of the deformities.
Fig. 4. Stainless steel bars were used to support the ster-
num in three patients with very extensive resection of the
costal cartilage.