CARDIOVASCULAR JOURNAL OF AFRICA • Vol 24, No 8, September 2013
316
AFRICA
Discussion
Until recently, conventional treatment for insufficiency of
the GSV was ligation over the saphenous–femoral arch and
stripping of the GSV. However this surgical operation has a long
postoperative recovery time, a high incidence of postoperative
paresthesias, haematoma formation and pain, a high recurrence
rate, and is associated with wound-related complications such
as infection.
8,9,14,15
Understanding the pathophysiology of venous
insufficiency, and technological advancement have enabled
minimally invasive methods to be used for ablation of the GSV.
RF consists of electric and magnetic waves that transform into
thermal energy after contact with tissue.
16
The increased luminal
temperature induces vein wall contraction via denaturation of the
collagen matrix. Various macro- and microscopic changes occur,
including endothelial destruction, shortening and thickening of
the venous wall and fibrotic sealing of the vessel lumen.
16,17
Lohr
et al
. pointed out that the temperature gradient between the intima
and adventitia and duration of the time of heating determines the
total injury to the vein wall collagen and subsequently the total
shrinkage of the vein wall.
11
Earlier studies using first-generation RF devices and
catheters
17,18
maintained a set point temperature of 90°C and
a slow incremental pull-back catheter technique with a speed
of 2–3 cm/min. Merchant
et al
.
19
pointed out the importance
of the pull-back speed and its effect on the success of the
venous closure. They also reported a higher incidence of clot
formation, early vessel recanalisation and thermal injury with
this technique.
19
These issues are not considered to be relevant
with the development of the latest generation catheters such as
ClosureFast.
Kapoor
et al
. retrospectively analysed the data of 100 patients
treated with ClosureFast and showed that the new technique
offsets the limitations of previous RF techniques, leads to good
venous closure with minimal complications and improves patient
comfort.
20
This was the reason for us using the latest generation
catheter in our study.
The ClosureFast catheter treats a 7-cm segment of vein,
providing an improved segmental contact with the vessel wall
and has a lubricious jacket to ease guidance and decrease the
formation of clotting.
17
There is a temperature sensor near the
catheter tip. The RF generator provides transmural heating of
the venous wall and limits heating up of the surrounding tissue
by using minimum energy (15–40 W) to reach and maintain a
temperature set point of 120°C during the 20-s cycles.
11,16
Tumescent anaesthesia isolates the GSV from the surrounding
soft tissue and by creating a heat sink, it prevents transfer of
the thermal effects of intravascular energy to non-target tissues.
Furthermore, it mechanically decreases the luminal diameter
of the vein to better contact the laser or RF catheters, and
drains the blood from inside the lumen to decrease thrombus
formation.
11,12,21
Merchant
et al
. showed a reduction in the incidence of
paresthesia and rate of skin burn after the use of tumescent
infiltration.
22
However, it increases the operation time, its
placement requires multiple patient needle-sticks, causing
brusing, and it is the most difficult part of the learning curve.
12
Besides Gibson
et al
. drew attention to the difficulty of adjusting
the correct amount of tumescent solution.
23
Technological
advances in RF catheters have decreased the risk of pain,
bruising and thermal injury to the nerve, muscle or skin.
The aim of our study was elimination of tumescent infusion.
Avoiding tumescent anaesthesia in group 2 reduced the ablation
time significantly, as expected. Most importantly, however,
the primary closure rates were similar at six months and no
significant difference was found between the groups in terms
of VAS and ecchymosis scores, postoperative measured GSV
diameters, and the time needed to return to daily activities.
The great saphenous nerve is very close to the GSV below
the knee. We aimed to avoid nerve injury by performing venous
puncture above the knee. With the technological advantages of
the ClosureFast catheter, we did not encounter paresthesia in the
tumescentless group.
Our technique included external compression with ice and
dampening of the skin with saline (+4°C), thereby cooling the
skin and providing local hypothermia to prevent skin burn. In
group 1, we used tumescent anaesthesia. No skin burn was found
in either group.
RFA of the GSV with a diameter greater than 12 mm has
been another controversial issue, especially for first-generation
catheters. Manfrini
et al
. reported that tumescent anaesthesia
has a critical role to play in improving venous closure rates by
compressing the vein wall into close contact with the catheter.
24
Merchant
et al
. treated 59 limbs with GSV diameters greater than
12 mm and reported an occlusion rate of 96% at six months.
22
ClosureFast fits through a 7-Fr sheath, improving the segmental
contact with the vessel wall. Proebstle
et al
. treated 252 GSV
with ClosureFast with diameters as large as 18 mm.
25
They used
tumescent anaesthesia and the primary venous closure rate was
99.6% at six months. Calcagno
et al
. retrospectively analysed
338 patients and concluded that vein diameter exceeding 12
mm had no effect on closure rate with the ClosureFast catheter,
and using tumescent anaesthesia should allow for the succesful
treatment of large veins.
26
We did not find any reports investigating the effect of
ClosureFast without tumescent anaesthesia on vein diameters
>
12 mm. The mean diameter of GSV was 9.2 mm but the range
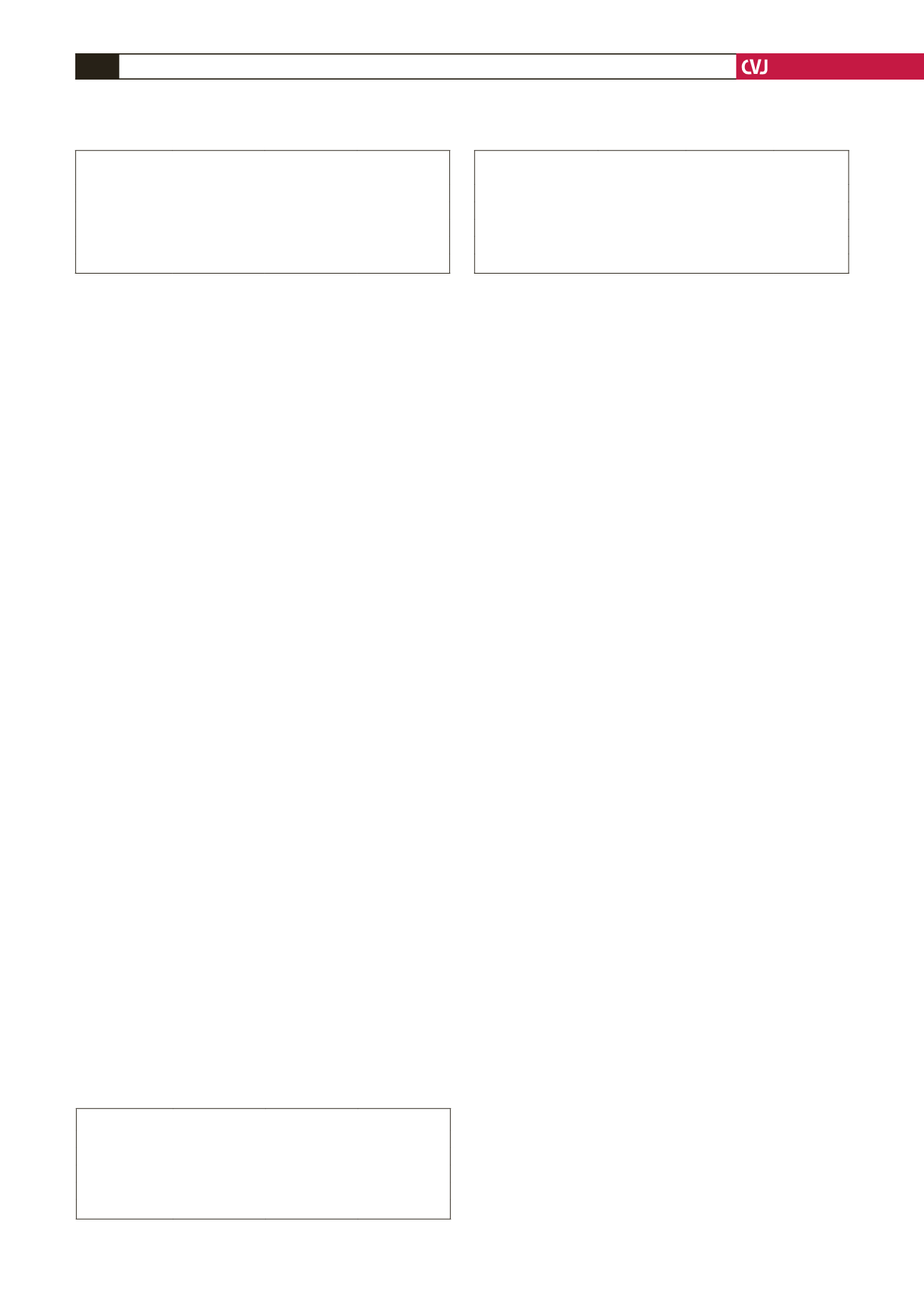
TABLE 4. POSTOPERATIVE ECCHYMOSIS SCORES OF THE PATIENTS
Postoperative time
Group 1
Group 2
p
-value
3rd hour
0 (0–2)
0 (0–3)
0.405
7th day
0 (0–0)
0 (0–0)
1.000
1st month
0 (0–0)
0 (0–0)
1.000
6th month
0 (0–0)
0 (0–0)
1.000
TABLE 5. DIAMETER OF GSVAT SFJ ANDABOVE THE KNEEAT
ONE-MONTHAND SIX-MONTH DOPPLER ULTRASOUND FOLLOW UP
Diameter of GSV (cm)
Group 1
Group 2
p
-value
1st month above the knee 4.2 (0.0–10.5)
4.2 (2.7–10.5)
0.753
1st month at SFJ
8.3 (4.7–21.7)
8.4 (4.1–22.1)
0.480
6th month above the knee
3.5 (2.4–8.8)
3.7 (2.2–8.1)
0.960
6th month at SFJ
7.0 (3.8–18)
7.0 (3.8–20.1)
0.971
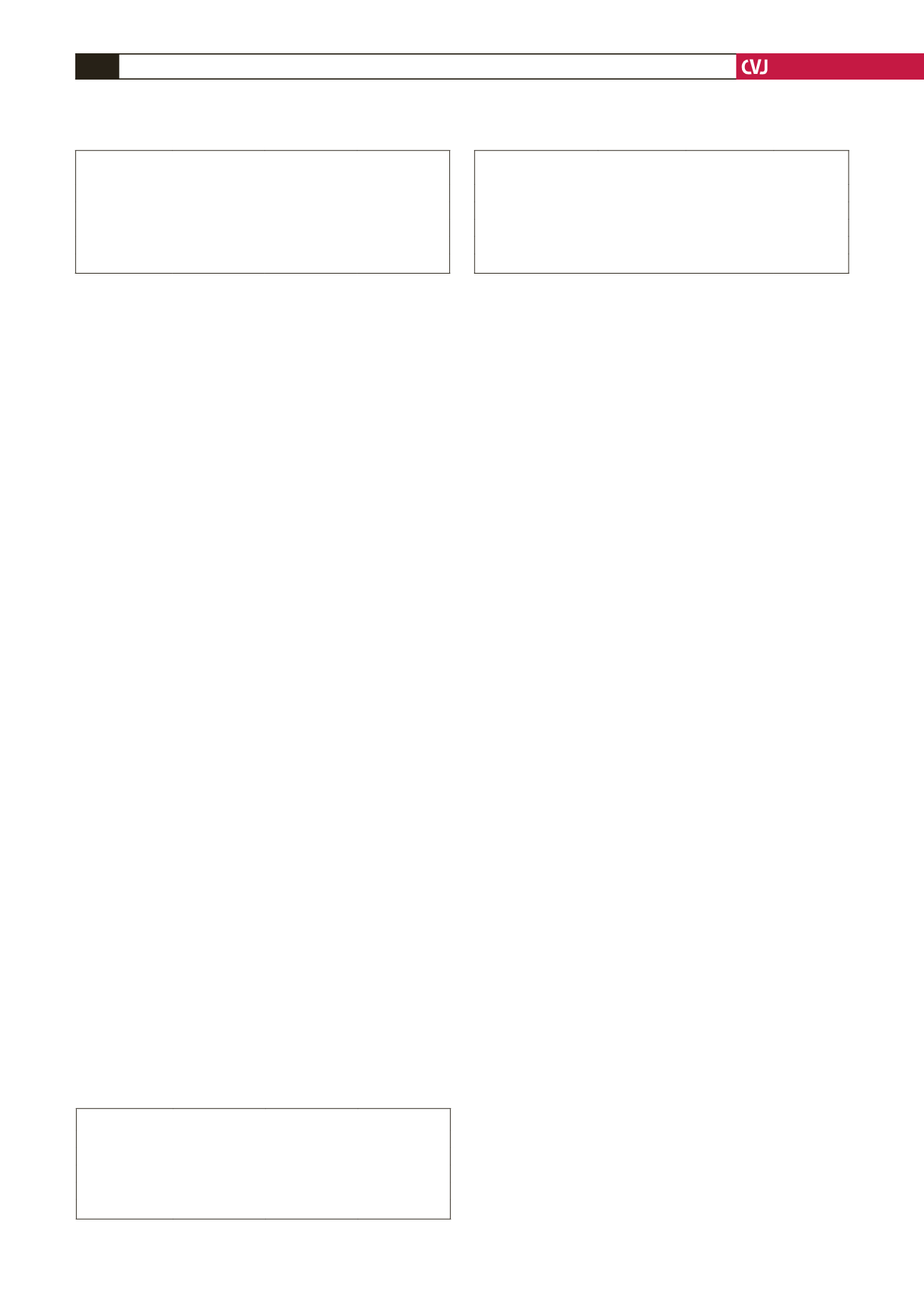
TABLE 3. POSTOPERATIVEVISUALANALOGUE SCALE
SCORES OF THE PATIENTS
Postoperative time
Group 1
Group 2
p-value
3rd hour
2 (0–7)
2 (0–8)
0.231
7th day
0 (0–1)
0 (0–1)
0.189
1st month
0 (0–5)
0.5 (0–6)
0.105
6th month
0 (0–1)
0 (0–1)
1.000