
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 2, March/April 2015
AFRICA
75
requirements during operative surgery, the attractiveness is
evidenced by a shorter hospital stay, and access to a lesion from
a remote site free of contamination. The long-term durability of
this form of intervention is unknown at present.
Prognosis and outcome
The laboratory features are characterised by deranged CD4
counts, hyperglobulinaemia, inverted CD4/CD8 ratios and hypo-
albuminaemia.
29,31,47
Van Marle
et al
.
47
attempted to correlate
some of these parameters to surgical outcome and revealed that
these markers were associated with a poorer prognosis, while
Robbs and Paruk
4
failed to demonstrate a correlation.
Peri-operative mortality rates have ranged from 9–10.6% in
South Africa
4
to 33% in Houston,
57
where the majority (56%) of
patients were intravenous drug abusers with challenges related to
wound healing and sepsis. Lin
et al
.
57
reported a late graft sepsis
rate of 10% with prosthethic graft usage.
The long-term results are largely unknown as follow-up
remains a problem. Furthermore, the majority of the reported
cases were conducted in the pre-HAART era.
Occlusive disease
Occlusive disease is a less studied entity that shares microscopic
and laboratory features with its aneurysmal counterpart. It has
an affinity for young males under 40 years of age. The limbs are
usually involved, with the lower limbs involved more frequently
than the upper limbs.
3,4,47,48,58-60
The classic risk factors for occlusive
vascular disease are less prevalent.
46,58
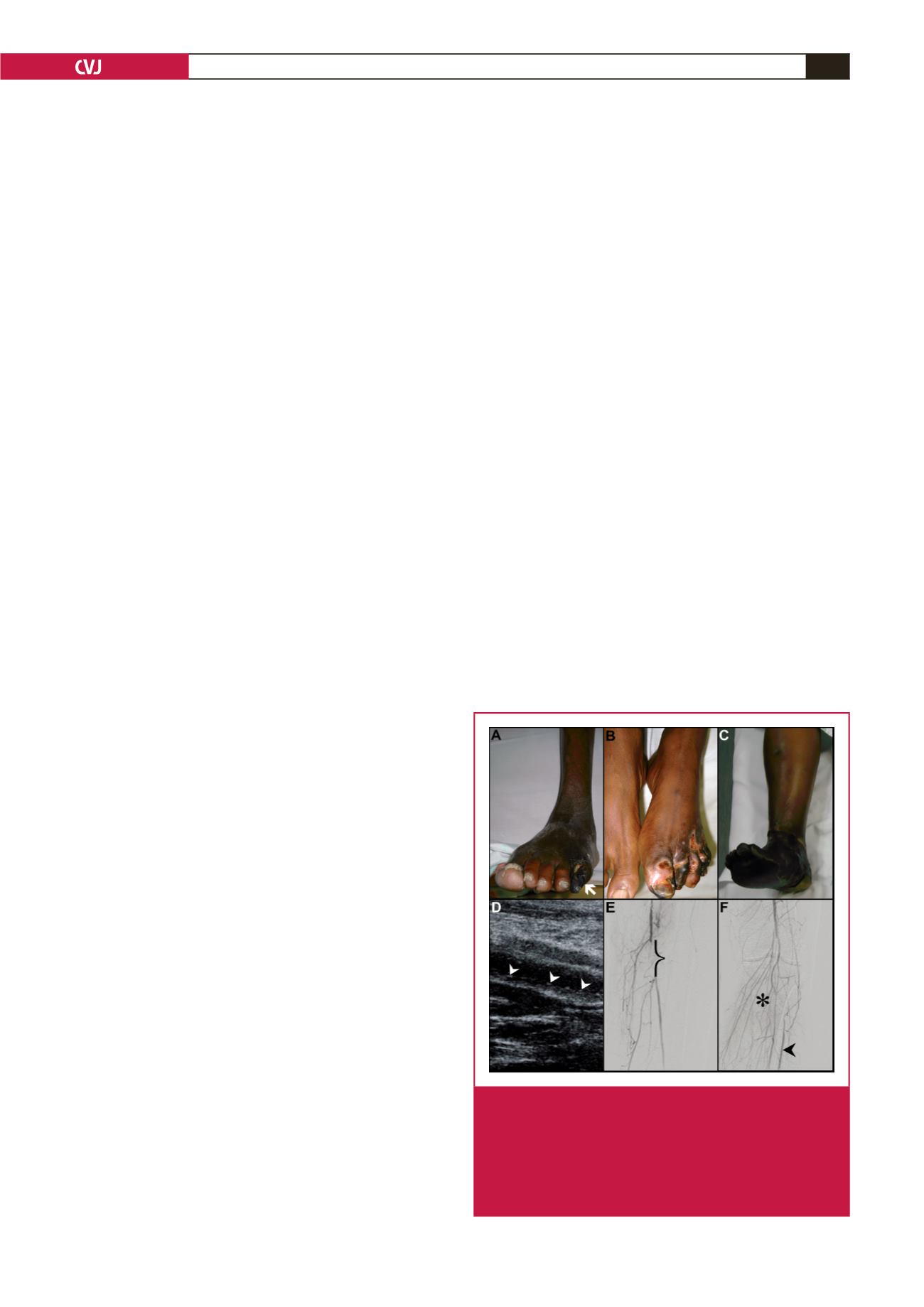
Clinical manifestations
Patients may manifest acutely with primary thrombosis and
clinical features of acute arterial occlusion. Chronic disease may
present with features of critical ischaemia in the form of rest
pain or gangrene in more than 50% of patients (Fig. 5A–C).
Anatomically, infra-inguinal disease is more common than
aorto-iliac disease.
Imaging studies
Duplex studies have demonstrated typical linear sub-intimal
deposition of calcium in the vessel wall, classically described
as a ‘string of beads’
32
appearance (Fig. 5D), together with
evidence of intraluminal thrombus in patients presenting acutely.
Mulaudzi
et al
.
22
documented that additional imaging in this
group of patients was non-contributory.
Invasive imaging using computed tomographic studies and
angiography have shown that the contralateral vessels are usually
disease free while the symptomatic limb vessels demonstrate
multi-segment involvement, long-segment occlusions (Fig.
5E), poor distal run-off and an abundance of well-established
collaterals (Fig. 5F).
3,4,47,48,58,59
Pathology
In the series by Mulaudzi
et al
.,
22
36% of patients (
n
=
8)
who had histopathological investigations had organised bland
thrombus and an intense inflammatory reaction in the vessel
lumen. On microscopic analysis of the occlusive lesions, medial
scattered chronic inflammatory cells, focal medial calcification,
destruction of the internal elastic lamina (Fig. 6A) and medial
muscle, leucocytoclastic vasculitis of the vasa vasora (Fig.
6B), mural fibrosis (Fig. 6C) and luminal organising thrombus
(Fig. 6A) have been noted. In addition, viral proteins on the
lymphocytes of arterial and aneurysmal tissue were seen but
atherosclerosis was not identified.
Nair
et al
.
59
found no evidence of atherosclerotic involvement of
the vessel wall during macroscopic examination at surgery. Autopsy
studies performed by Micheletti
et al
.
61
on donor coronary vessels
of 10 HIV-positive patients revealed linear calcium deposition in
the internal elastic lamina, independent of intimal atherosclerosis
and calcification, a microscopic feature supposedly unique to
HIV-infected individuals. This feature is theorised to reflect arterial
stiffening and may be associated with premature vascular aging
and chronic illness in HIV-infected patients.
Management
The management of HIV-infected patients who present with
vascular pathology is congruent with the standard guidelines
of HIV-naïve patients, with conservative management being
reserved for patients with full-blown AIDS.
3,4,47,48,58
Those patients
presenting with acute arterial occlusion as a result of primary
thrombosis are characterised by unfavourable outcomes with
embolectomy. This is borne out in the study by Mulaudzi
et
al
.,
22
who demonstrated that embolectomy was often followed by
re-thrombosis within 48 hours. In his study, 17/22 patients were
treated by ablation, with a limb salvage rate of 27%.
22
A possible
reason for the poor outcome was explained by the persistence
of the underlying vasculitic process despite management of the
obstructing lesion.
Patients with chronic disease are imaged and treated with
surgical bypass, catheter-directed therapy, or an ablation for
Fig. 5.
Clinical presentation of HIVocclusive disease:gangrene
of the fifth digit (A, arrow); left forefoot (B); and entire
foot (C). Duplex image of the superficial femoral artery
(D), demonstrating a ‘string of beads’ pattern (arrow-
heads). Angiogram demonstrating left femoro-popliteal
disease with occlusion (E, bracket), poor distal run-off
(F, arrow), and abundant collaterals (F, *).

















