
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 2, March/April 2015
72
AFRICA
that there was thinning of the arterial media. Although this
observation may be indicative of a significant pre-clinical stage
towards HIV-associated vasculopathy with resultant vessel wall
weakening, it has to be interpreted with caution in view of study
limitations in terms of numbers, lack of information on HAART
and duration of HIV infection.
The entry of the virus into the cell triggers release of
tissue factor 2, which induces thrombosis and chemokine c-c
motif ligand (CCL-2) production. This is instrumental in
promoting atherogenesis. These observations may support a role
for direct viral invasion, and may contribute to knowledge on
the thrombotic complications and coronary events experienced
by HIV-infected patients.
‘Molecular mimicry’
Tilson
21
studied an HIV-related carotid aneurysm and explains
molecular mimicry whereby HIV viral proteins share antigens in
the wall of the vasculopathic process. The load-bearing matrix
of the arterial wall is composed of an artery-specific antigenic
protein (ASAP), matrix cell adhesion molecule-1 (Mat-CAM-1).
It is theorised that the virus and its toxic by-products share ligands
that are characterised by DNA sequence similarities between the
ASAP and viral envelope glycoprotein, gp41 and gp120.
21
This
may potentially result in autoimmune-mediated cell damage
during infection. However, no similarities were found between
Mat-CAM-1 and HIV envelope glycoproteins in this study.
Therefore an alternate explanation proposed is that of direct viral
invasion of the aortic fibroblasts at the level of the adventitia.
21
Thrombophilic screening
While the pathogenesis of occlusive disease is presently unclear,
thrombophilic screens have been sporadically performed with
regard to protein S, protein C and antithrombin III. Mulaudzi
et al
.,
22
however, found negative thrombophilic screens in 10
patients with primary arterial thrombosis in the acute setting.
Chronic infection in HIV-infected patients results in endothelial
injury and associated dysfunction. This sequence of events
culminates in atherosclerosis and thrombosis.
Experimental models
Animal models
23
have been employed to simulate the arterial
wall pathology in order to improve insight into the underlying
mechanisms of HIV-associated vasculopathy. Studies conducted
in transgenic mice infected by the HIV-1 provirus have
demonstrated an adventitial mixed inflammatory cell infiltrate,
medial hypocellularity and intimal hyperplasia following smooth
muscle migration, with sparing of the endothelial cells. The
intimal thickening produces intraluminal narrowing of some
vessels causing distal tissue ischaemia.
In addition, viral components have been observed in SMCs,
which in some instances have proliferated in the absence of
inflammation. This model partially explains the findings
in human arterial wall samples, with the key feature being
endothelial dysfunction. Although this model highlights the
conceptual principles of viral invasion, extrapolation of the
pathophysiological findings of arterial wall studies to the human
scenario remains challenging.
Current descriptions of HIV-associated
vasculopathy
Aneurysmal disease
Since the first report of
Salmonella
-related mycotic aneurysmal
disease by Du Pont
et al.
24
in an HIV-positive patient in 1989,
increasing numbers of reports have emanated from Zimbabwe,
Zambia and South Africa,
4,25-31
confirming the occurrence of
aneurysmal disease independent of bacterial infection. These
aneurysms are multiple, with a predilection for young individuals
and atypical locations, including the aorta, carotid, popliteal and
femoral vessels.
28,29,31
More recently, a predilection for femoral
artery involvement has been documented.
4
These aneurysms
occur in the advanced stages of HIV disease, as demonstrated by
low CD4 counts and systemic clinical features.
3,4
Clinical manifestations
Patients with aneurysms can be asymptomatic. However,
when presenting as a space-occupying lesion, the clinical
features are governed by the rate of growth, expansion and
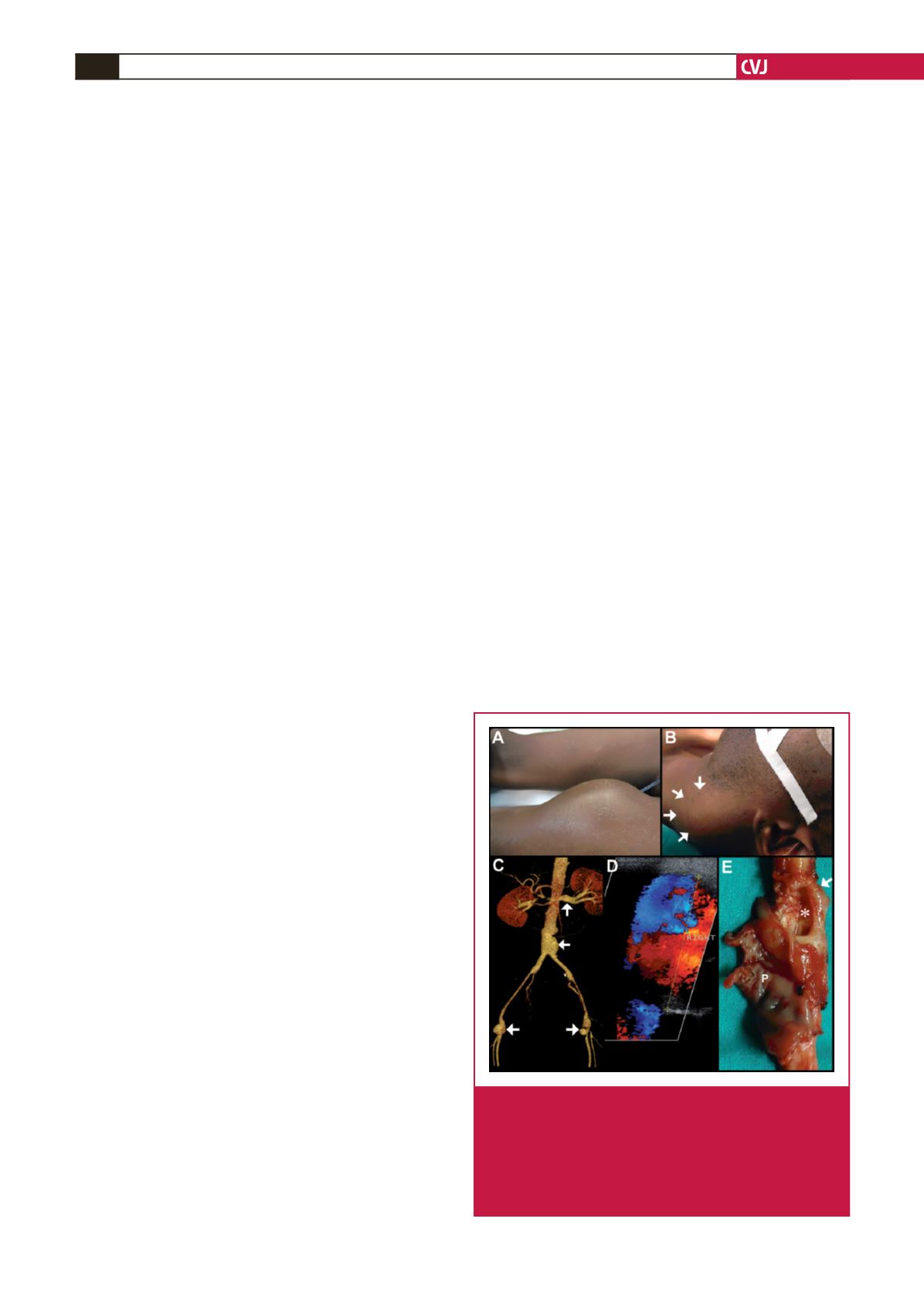
anatomical location. The presence of a pulsatile mass (Fig.
2A) may be complemented by constitutional findings of
weight loss, associated lymphadenopathy and/or the presence
of opportunistic infections. The symptom complex entails a
varying spectrum, from pain in the majority of patients, to the
associated effects of mechanical compression. An expanding
carotid aneurysm (Fig. 2B) may result in dysphagia, stridor,
hoarseness of voice, cranial nerve palsies, a hemispheric event
as a consequence of thrombo-embolisation or frank aneurysmal
rupture producing haemodynamic instability. Peripheral
Fig. 2.
Clinical presentation of HIV-aneurysmal disease: mass
in the left anterior thigh (A), and left neck (B, arrows).
CT angiogram demonstration of multiple aneurysms
in various anatomical locations (C, arrows). ‘Yin-yang’
sign demonstrated on the right common femoral artery
(D). Gross demonstration (E) of aneurysm (arrow) with
a ‘blow-out’ (*) and pseudo-aneurysm (P) formation.

















