
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 2, March/April 2015
AFRICA
71
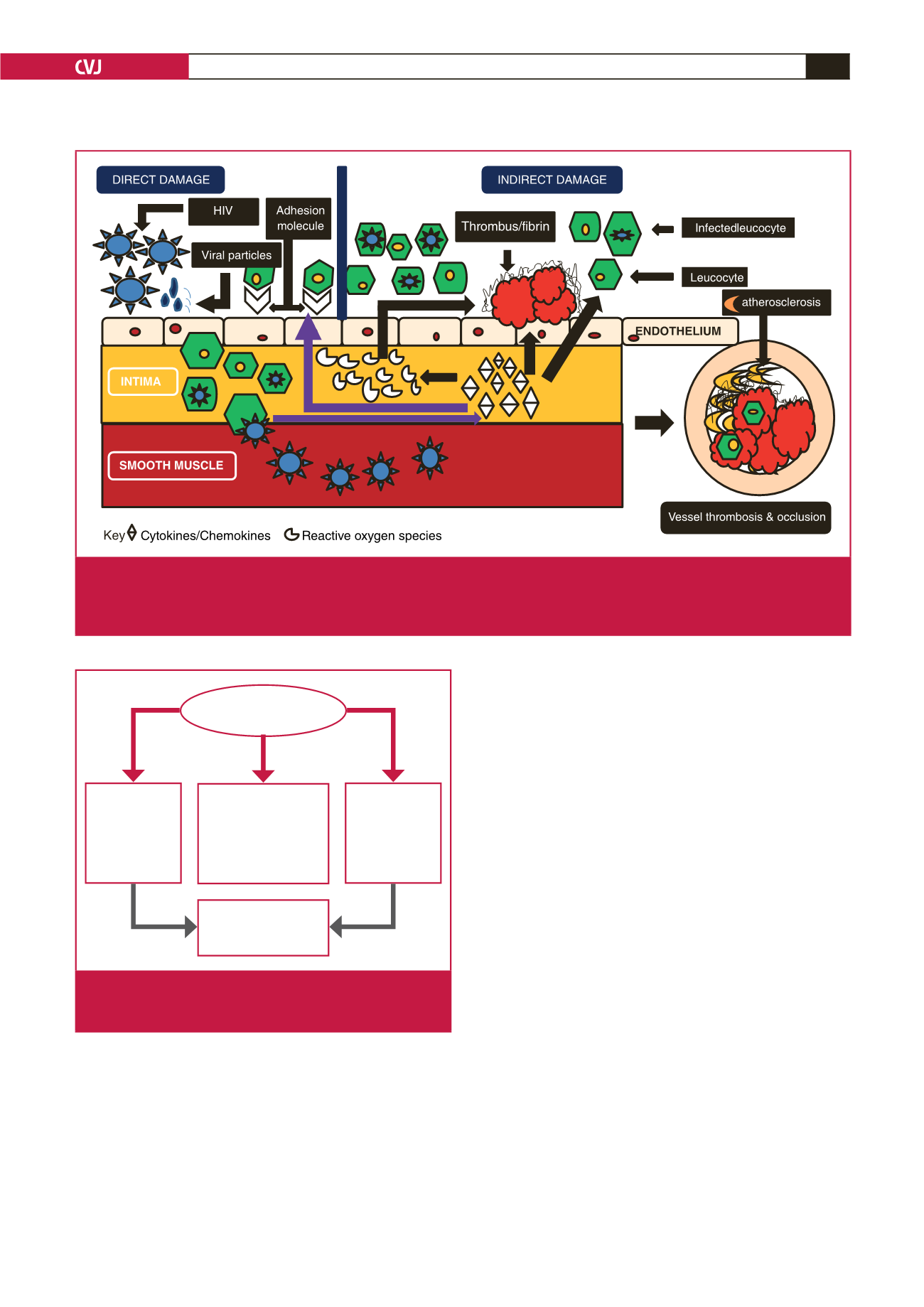
HIV-related endothelial dysfunction, incorporating a complex
interplay between cytokines and inflammatory components, has
been proposed.
14
The theoretical basis of this includes continuing
viral infection and associated viral protein toxicity leading to
vascular wall injury, an increase in viral load associated with the
release of interleukin 1 (IL1), interleukin 6 (IL6), interleukin
8 (IL8) and tumour necrosis factor-
α
(TNF-
α
), in conjunction
with immune activation and immune reconstitution as a result
of HAART.
14
This has been observed by Nieuwhof
et al.
15
who postulated
increased T-cell numbers associated with elevated CD25-positive
receptors in the setting of cerebral vasculitis. This theory is
supported by the response to steroids and daclizumab, a human
immunoglobulin G-K recombinant antibody that binds to
CD25.
15
It is thought that the HIV-transactivator of transcription
protein,
tat
, triggers inflammatory pathways that result in the
production of cytokines and adhesion molecules. A viral envelope
glycoprotein component (gp120) is a catalyst that stimulates
production of pro-inflammatory mediators, which target
endothelial cells.
14,16,17
Evidence from studies on flow-mediated
vasodilatation demonstrates that HIV-associated endothelial
dysfunction is catalysed by these cytokines and the inflammatory
process.
13,14,17
Role of smooth muscle cells
Smooth muscle cells (SMCs), the major cellular component of
the arterial muscularis media, have proliferative and migratory
potential. Key surface receptors, CD4, CCR5 and CXCR4,
render SMCs an ideal infective target that facilitates entry of the
HIV-1 viral components.
18
Viral invasion results in thinning of
the medial layer and sub-intimal aggregation of SMCs. Entry of
the viral envelope proteins may activate tissue factor 2, which is
a potent stimulant for the coagulation cascade.
While the SMCs seems to play a central role in arterial wall
pathophysiology, as evidenced by
in vivo
and
in vitro
SMC
studies,
19
this aspect of smooth muscle involvement has not
been studied in depth. More recently Gutierrez
et al
.,
20
in their
appraisal of intracranial vessels from autopsy specimens in a
pilot study of 15 arterial wall samples from five patients, found
Fig. 1A.
Schematic illustration of direct and indirect endothelial damage. The former is characterised by viral endothelial invasion,
upregulation of adhesion molecules, generation of reactive oxygen species and varied cytokine and chemokine responses.
The latter encompasses continued viral invasion, generation of an inflammatory cascade that leads to a vicious circle of
endothelial injury, activation and remodelling, culminating in thrombosis and occlusion.
HIV-INDUCED ENDOTHELIAL
DYSFUNCTION
PERMEABILITY
• protein leakage
• encephalitis
INFLAMMATION
• vasculitis
• occlusive disease
• aneurysms
• arteriovenous fistula
• dissections
•
intimal hyperplasia
•
elastic fragmentation
•
thrombotic occlusion
PROLIFERATION
• Kaposi
sarcoma
Fig. 1B.
Schematic representation of the clinicopathological
manifestations arising from HIV-induced endothelial
dysfunction.

















