
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 26, No 2, March/April 2015
76
AFRICA
unsalvageable limbs. Post-operative wound healing and graft
sepsis is not unusual.
48
To overcome this shortcoming, van
Marle
et al
.
58
used silver-impregnated grafts for surgical bypass.
Immediate post-operative results were favourable.
Prognosis and outcome
Attempts have been made to correlate serum albumin and CD4
counts with postoperative outcome in these patients but the
results vary. Although a low CD4 count in association with hypo-
albuminaemia correlated with a poor postoperative outcome,
58
the overall 30-day mortality rate for acute and chronic occlusive
disease attained by Robbs and Paruk
4
was 23%, compared to a
long-term mortality of 28.75% by van Marle
et al
.
58
Furthermore,
improved long-term survival in this grouping was negated by
poor limb-salvage rates of 36.1%, with poor distal run-off being
a contributory factor that precluded surgical bypass.
58
Other HIV-associated vascular manifestations
Spontaneous arteriovenous fistulae
Arteriovenous fistulae may occur as a result of trauma or
endovascular procedures. Spontaneous arteriovenous fistulae
following HIV infection are rare, with anecdotal experiences
reported in the literature.
48,62
A case report detailing this clinical
scenario related to a young patient presenting with a pulsatile
mass of his right lower thigh.
62
Angiography revealed a distal
superficial artery lesion with pooling of contrast and delayed
venous filling. The patient was treated surgically, with a successful
outcome. Microscopy of the arterial wall with regard to the
index patient demonstrated features similar to that observed in
aneurysmal and occlusive disease.
Spontaneous cervical artery dissection
An isolated case report described a spontaneous cervical artery
dissection.
63
This pathology was observed in the vertebral
artery. The speculated pathogenesis was a structural defect
in the arterial wall. Deficiencies of micronutrients, folate and
cobalamine have been observed in HIV-infected patients.
63
These
deficiencies result in high circulating homocysteine levels that are
thought to adversely affect the elastin content of the vessel wall,
rendering it potentially vulnerable to a dissection.
Atherosclerosis in HIV-infected patients
Evidence demonstrates that endothelial injury in HIV-infected
patients occurs as a result of progression and severity of HIV
infection
per se
.
14
However, more recently, atherosclerosis has
been documented following HIV infection and its management
with HAART.
64-70
The relationship between atherosclerosis and HIV
infection
Atherosclerotic disease is essentially an inflammatory event
in the setting of classic cardiovascular risk factors, namely,
smoking, hyperlipidaemia, family history, diabetes and
hypertension. Accelerated atherosclerosis may evolve from
the metabolic changes accompanying HIV infection, inclusive
of hypercholesterolaemia, decreased high-density lipoprotein
(HDL) cholesterol, elevated C-reactive protein levels and
increased fibrinogen and plasminogen-activating inhibitor
activity. Patients with these metabolic changes are more prone
to coronary artery disease.
64,65
In addition, cigarette smoking is a
contributory factor.
70
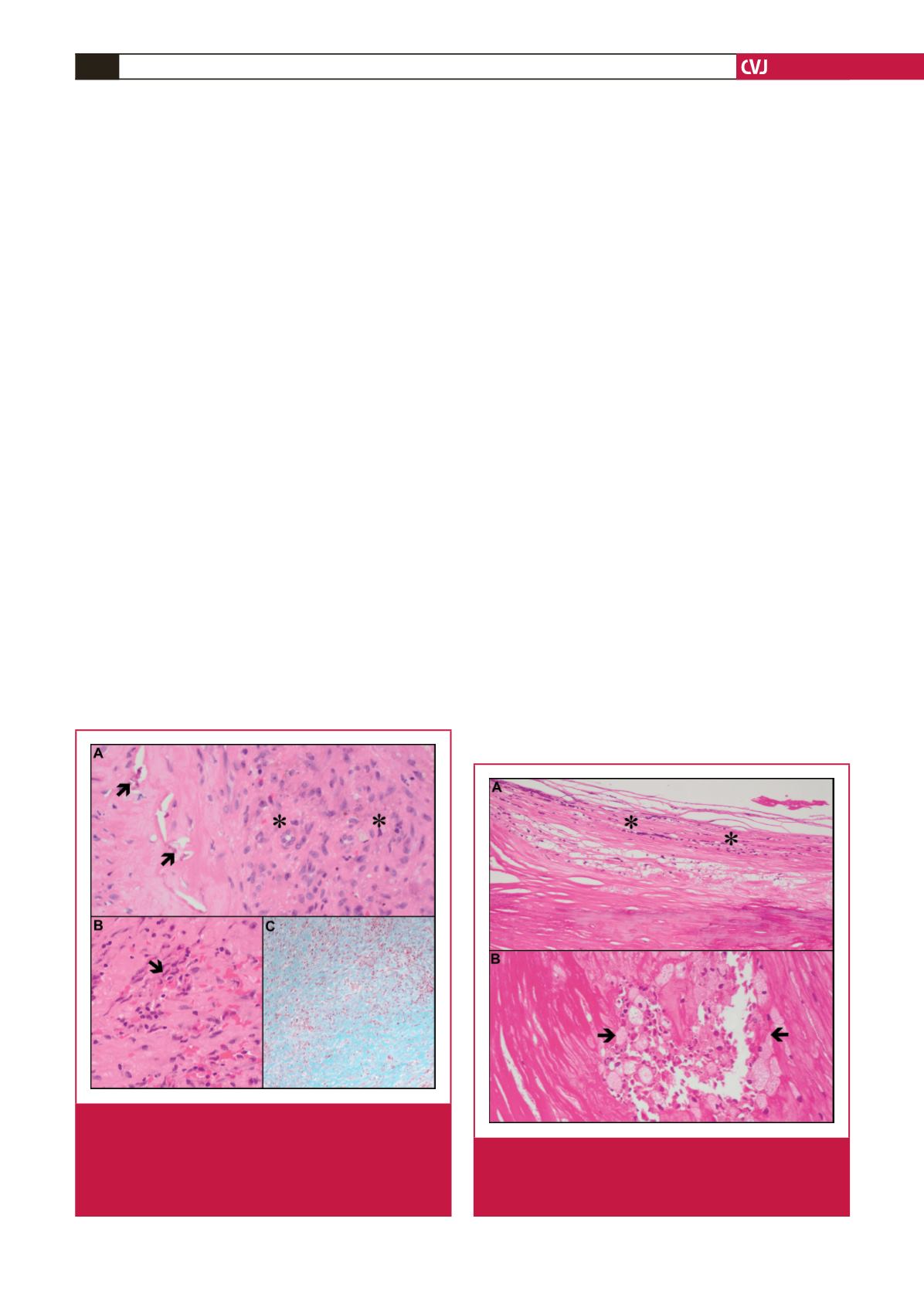
Fig. 6.
Histopathology of occlusive HIV disease: internal elas-
tic lamina damage (A, arrows) and organising luminal
thrombus (A, asterisks) (haematoxylin and eosin,
240
×
); leucocytoclastic vasculitis (B, arrow) (haema-
toxylin and eosin, 240
×
);
and medial and adventitial
fibrosis (C)
(Masson trichrome, 240
×
).
Fig. 7.
Aneurysm from a patient on antiretrovirals with the
metabolic syndrome: intimal inflammation (A, aster-
isks) (haematoxylin and eosin, 240
×
);
and foam cells
(B, arrows) (haematoxylin and eosin, 240
×
)
.

















