
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 2, March/April 2017
AFRICA
121
was not statistically significantly different between the groups
(
p
=
0.57), while at three years, the intergroup difference was
statistically significantly different (
p
=
0.01).
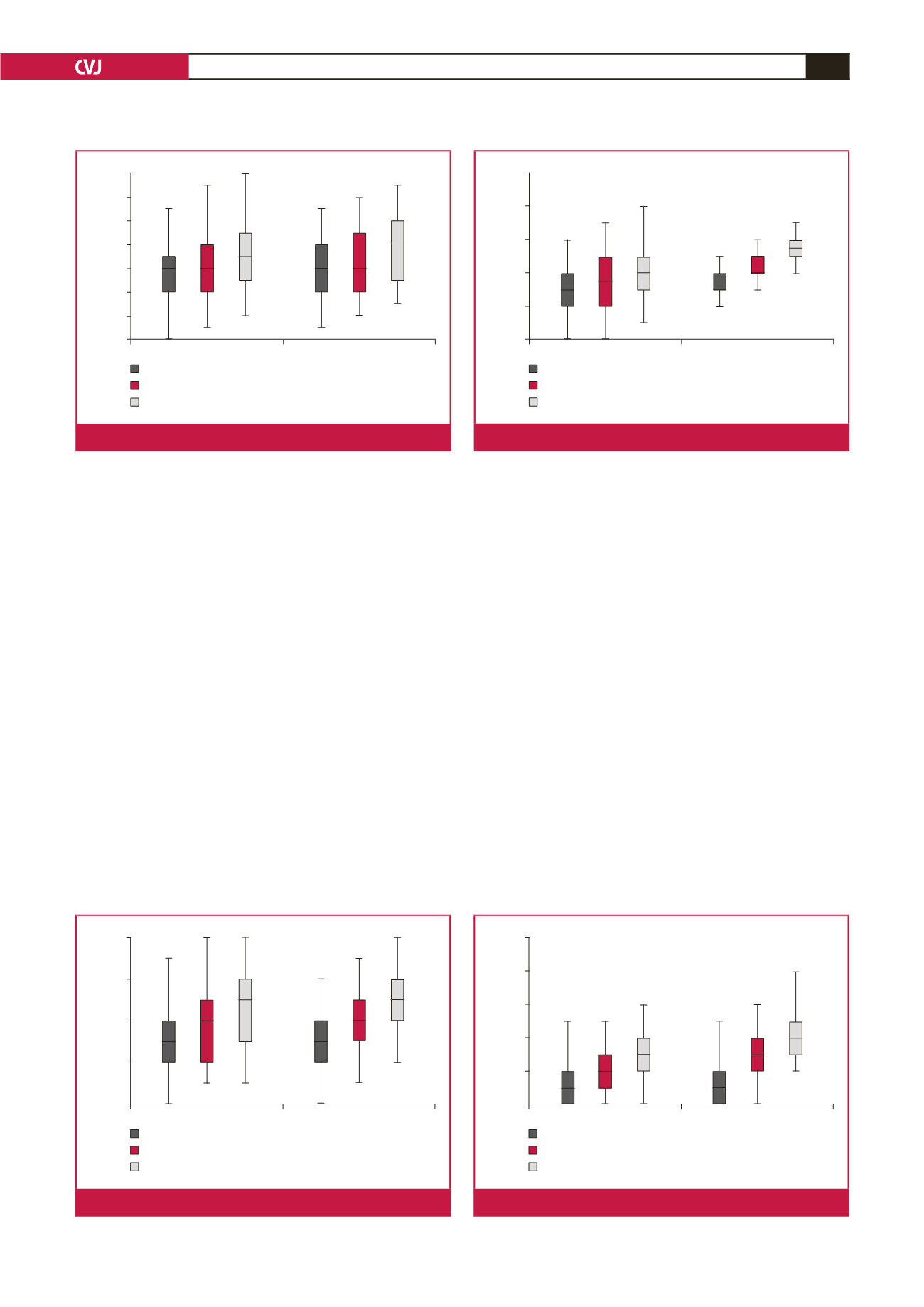
Pre-operatively at the level of the sinotubular junction,
the mean aortic diameters were not significantly different
between the groups (Fig. 3) (
p
=
0.08), while the mean aortic
diameters at one and three years postoperatively were statistically
significantly different between the groups (
p
=
0.002 and
p
=
0.0001, respectively). Annual increase in diameter was extremely
significantly different between the groups (
p
=
0.0001 and
p
=
0.0001, respectively). Mean annual difference in diameter was
found to be extremely significantly different between the groups
(
p
=
0.0001 and
p
=
0.0001, respectively).
Pre-operatively, mean aortic diameters measured at the level
of the tubular ascending aorta were not significantly different
between the groups (Fig. 4) (
p
=
0.79). However, mean aortic
diameters measured one and three years postoperatively were
extremely significantly different between the groups (
p
=
0.0001
and
p
=
0.0001, respectively). The increase in diameter of the
ascending aorta was extremely significantly different in both
groups (
p
=
0.0001 and
p
=
0.0001, respectively). Intergroup
differences in mean value of the diameter of the ascending
aorta at one and three years postoperatively were extremely
significantly different (
p
=
0.0001 and
p
=
0.0001, respectively).
Discussion
Since proximal anastomosis of the coronary artery graft to the
ascending aorta requires aortotomy, aortic integrity is disrupted
during this procedure. Besides, coronary artery grafts in their
new position will increase the haemodynamic workload of the
ascending aorta and, theoretically, they can be seen as a cause
of aortic dilatation. However, no clinical or experimental study
in the literature has held coronary artery grafts responsible for
aortic dilatation.
We could also not find any study in the literature evaluating
the relationship between mid- and long-term increase in aortic
diameter and proximal anastomosis performed on the ascending
aorta in patients with aortic dilatation who did not require
surgical intervention but underwent CPB and isolated CABG. We
searched for the words ‘aortic dilatation’, ‘proximal anastomosis’
and ‘coronary artery bypass grafting’ in the English literature
of PubMed, but could not find any article related to this topic.
No study could be found in the literature referring to
aortic dilatation caused by aortic side clamping. Therefore no
assessment was done in our study on the effects of aortic side
clamping versus aortotomy. New studies are needed to determine
whether there is a difference. We rarely undertake proximal
anastomosis to the aorta using the aortic cross-clamp, we prefer
the aortic side-clamp.
Aortotomy absent
Aortotomy present
32
30
28
26
24
22
20
18
Post-operative first year aortic annulus diameter
Pre-operative aortic annulus diameter
Post-operative third year aortic annulus diameter
Diameter (mm)
Fig. 1.
Measurements of the aortic annulus.
Aortotomy absent
Aortotomy present
42
40
38
36
34
Post-operative first year sinus valsalva diameter
Pre-operative sinus valsalva diameter
Post-operative third year sinus valsalva diameter
Diameter (mm)
Fig. 2.
Measurements of the sinus of Valsalva.
Aortotomy absent
Aortotomy present
46
44
42
40
38
36
Post-operative first year SJT diameter
Pre-operative SJT diameter
Post-operative third year SJT diameter
Diameter (mm)
Fig. 3.
Measurements of the sinotubular junction.
Aortotomy absent
Aortotomy present
50
48
46
44
42
40
Post-operative first year ascending aortic diameter
Pre-operative ascending aortic diameter
Post-operative third year ascending aortic diameter
Diameter (mm)
Fig. 4.
Measurements of the ascending aorta.

















