
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 2, March/April 2017
AFRICA
123
(Table 3). However, during the three years of follow up, only a
minimal contribution of COPD to aortic dilatation at the level
of the sinus of Valsalva was detected (Table 3). In patients with
diabetes, the expansion velocity was observed to be 0.4 mm/year,
being most marked at the level of the sinotubular junction.
Hypertension is known to be an independent risk factor
for aortic dilatation. In various studies, annual increases in the
diameter of the ascending aorta have been reported at 1.25 mm
in normotensive and 2.8 mm in hypertensive patients.
21
However,
since these patients are continually on drug therapy, it is difficult
to investigate the effects of uncontrolled hypertension on annual
expansion rates. In the presence of controlled hypertension and
diabetes, dilatation of the sinotubular junction and tubular
segments of the aorta was more frequently observed. In tractable
hypertension, annual dilatation rate at the level of the tubular
aorta was found to be 2.2 mm.
21
In our study, age demonstrated a significant correlation with
dilatation rates in both groups for all segments of the aorta,
excluding the aortic ring. Other risk factors made minimal
contributions to dilatation rates, with no statistically significant
differences (
p
>
0.05) (Table 3).
Various formulae have been developed to predict the
expansion rate of aortic aneurysms, but no correlation between
the determined and estimated size of the aneurysm could be
demonstrated.
22
Bonser
et al
. followed up the natural course of
aneurysms in their series and reported an annual aortic expansion
rate of 3.3 mm for 44-mm-dilated aneurysms associated with
thrombi, but without any evidence of stroke and TIA. The
annual expansion rate was 1.9 mm without the concurrent
presence of thrombi. In this series, decreased growth rates were
reported for larger aneurysms.
22
Similarly, segments proximal and distal to the aneuryms were
tracked in patients who had previously undergone aortic surgery,
and a decrease in expansion rate of the aneurysms to 1.18–1.59
mm/year was reported.
19
In our cases, annual expansion rates
differed in various aortic regions, while the tubular (mid-)
segment of the ascending aorta was the most dilated portion.
Irrespective of aetiological factors, the mean expansion rate of
this segment was 1.2
±
0.9 mm/year, which was similar to the
dilatation rate following AVR.
On TTE, measurements of the aortic diameter may
demonstrate individual differences. CT angiography has
a higher sensitivity and specificity for the ascending aorta.
However, in multi-slice sections, it is difficult to evaluate the
sinotubular junction and annulus. In addition to the higher
cost of CT angiography, the contrast material used carries
risks of anaphylaxis and renal toxicity. Therefore, we deemed
it appropriate to analyse our cases using TTE, which allows
evaluation of ventricular and valvular function.
Limitations
Pre-operatively, the aortic diameters of our patients ranged
between 40 and 45 mm. Since it is known that the expansion
rate decreases in proportion to the increase in aortic diameter,
we believe that comparative regression analysis between groups
of aortae with varying diameters would reveal a correlation.
Although our follow-up period was only three years, we obtained
values close to those cited in the literature. However, we are of
the opinion that in long-term follow-up studies (five to 10 years),
more significant and precise results would be obtained.
Genetic investigations were not done in our cases or in other
studies on this subject. When undertaking genetic investigations,
if patients with connective tissue disorders are grouped separately,
then the number of extreme values would decrease and these
groups would demonstrate a more homogenous distribution,
with similar effects on the outcomes.
Conclusion
In our three-year follow-up study on patients with ascending
aortic dilatation that did not require surgical intervention,
who underwent proximal anastomosis of the ascending aorta
and only CABG surgery, we detected significant increases
in diameters of the sinotubular junction and tubular aorta.
Since our study population was homogenous as far as the
demographic and clinical characteristics were concerned, and
their hypertension was under control, we believe that this
statistically significant postoperative increase in expansion rate
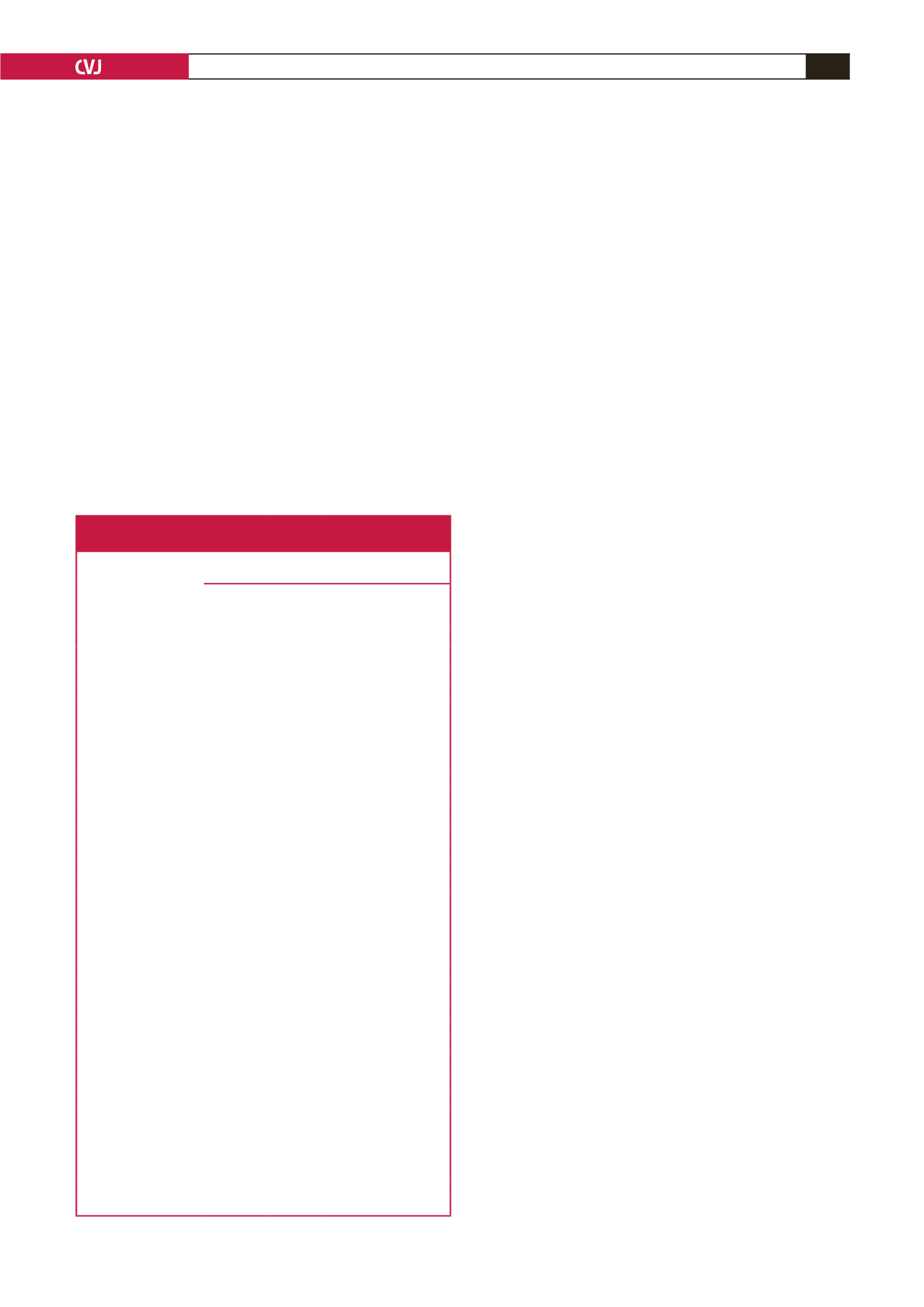
Table 3. The effect of pre-operative risk factors on changes in
aortic diameter at three years of follow up
Difference in diameter of the ascending aorta
(mm/3 years)
Aortic
ring
Sinus of
Valsalva
Sinotubu-
lar junc-
tion
Tubular
aorta
Hypertension
Present
1.27 ± 1.1 1.5 ± 0.37 1.5 ± 1.2 6.7 ± 1.9
Absent
1.1 ± 1.3 1.6 ± 0.38 1.1 ± 1.1 2.1 ± 1.7
p
-value
a
0.488
0.501
0.01
0.001
Smoking
Present
1.1 ± 1.2 1.6 ± 0.34 0.8 ± 1.0 3.7 ± 3.2
Absent
1.2 ± 1.3 1.5 ± 0.45 1.1 ± 1.1 3.3 ± 2.5
p
-value
a
0.756
0.163
0.004
0.793
Hypercholesterolaemia
Present
1.1 ± 1.3 1.6 ± 0.4 1.4 ± 1.2 3.0 ± 2.6
Absent
1.2 ± 1.2 1.6 ± 0.41 1.1 ± 1.0 3.7 ± 2.7
p
-value
a
0.852
0.401
0.222
0.97
Alcohol abuse
Present
0.75 ± 1.0 1.8 ± 0.3 1.1 ± 1.3 3.9 ± 3.0
Absent
1.2 ± 1.2 1.6 ± 0.4 1.2 ± 1.1 3.4 ± 2.7
p
-value
a
0.282
0.01186 0.745
0.540
Diabetes mellitus
Present
1.1 ± 1.2 1.7 ± 0.3 1.2 ± 1.1 3.3 ± 4.2
Absent
1.7 ± 1.7 1.6 ± 0.4 0.4±0.7 3.4 ± 2.6
p
-value
a
0.095
0.475
0.01
0.195
Chronic obstructive pulmonary disease
Present
1.5 ± 0.7 1.6 ± 0.4 1.4 ± 1.0 3.1 ± 1.9
Absent
1.1 ± 1.3 1.4 ± 0.3 1.2 ± 1.1 3.4 ± 2.7
p
-value
a
0.295
0.032
0.233
0.755
Gender
Female
1.3 ± 1.0 1.5 ± 1.2 1.3 ± 1.2 3.6 ± 2.0
Male
1.4 ± 0.9 1.4 ± 1.1 1.2 ± 1.1 3.5 ± 2.2
p
-value
a
0.752
0.252
0.920
0.178
Beta-blocker (+)
Present
1.2 ± 0.0 1.4 ± 1.2 1.3 ± 1.2 3.0 ± 1.9
Absent
1.3 ± 0.0 1.5 ± 1.1 1.2 ± 1.3 3.9 ± 2.1
p
-value
a
0.190
0.082
0.178
0.098
a
Mann–Whitney
U
-test.

















