
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 2, March/April 2020
AFRICA
73
baseline, peak inspiratory pressure (PIP), mean airway pressure
(mPaw), intrinsic positive end-expiratory pressure (iPEEP) and
dynamic lung complicance (DLC) were not different between
the sevoflurane and propofol groups (
p
=
0.795, 0.445, 0.608
and 0.486, respectively, by independent samples
t
-test). These
mechanical variables were similar in each group before CPB, at
15 min after declamping, and five, 30 and 60 min post-CPB (
p
=
0.625, 0.561, 0.326 and 0.342, respectively, by repeated measures
ANOVA).
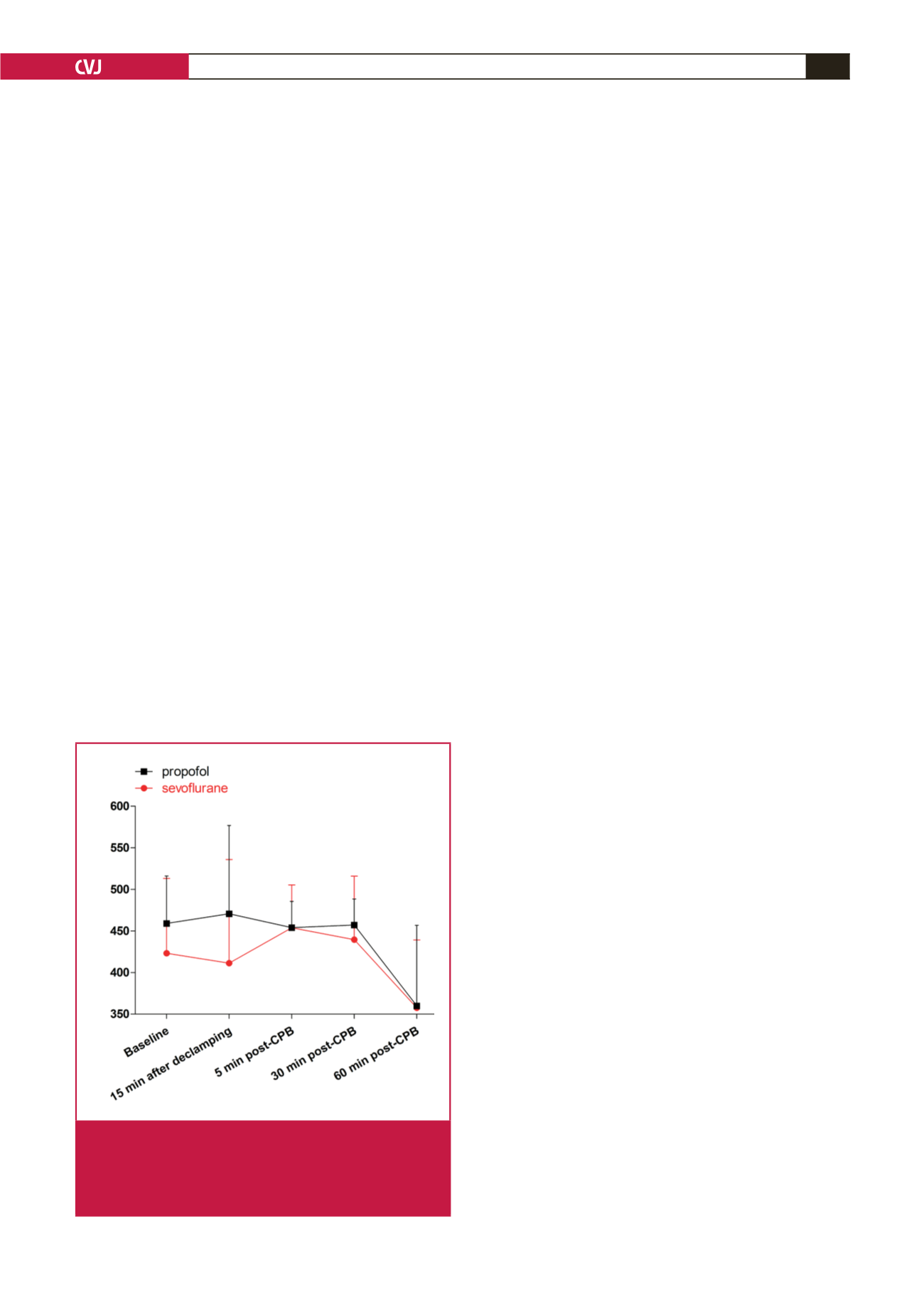
As shown in Fig. 1, PaO
2
/FiO
2
was not different between the
sevoflurane and propofol groups at baseline (423
±
90 vs 459
±
57 mmHg,
p
=
0.242 by independent samples
t
-test). There was
also no difference in PaO
2
/FiO
2
between the groups at 15 min
after declamping (411
±
125 vs 471
±
106 mmHg), and five (454
±
52 vs 454
±
32 mmHg), 30 (440
±
76 vs 457
±
31 mmHg) and
60 min (358
±
82 vs 360
±
97 mmHg) post-CPB (
p
=
0.477 by
repeated-measures ANOVA).
Discussion
Our study showed that there were no differences in PaO
2
/
FiO
2
, respiratory mechanics and haemodynamics during CPB
in patients undergoing cardiac valve replacement when a
sevoflurane- or propofol-based anaesthetic regimen was applied.
This is the first investigation to evaluate the difference in
oxygenation between an inhaled and intravenous anaesthetic
regimen in cardiac surgery with CPB.
The results of this study showed that the oxygenation
index of PaO
2
/FiO
2
was not significantly decreased (
>
400
mmHg at 15 min after declamping, and at five and 30 min
post-CPB, and ~ 360 mmHg at 60 min post-CPB) compared
with the respective baselines in the sevoflurane- and propofol-
based groups, indicating that lung injury was mild during the
early period of CPB in our patients undergoing cardiac valve
replacement surgery.
Volatile anaesthetics are frequently employed in cardiothoracic
surgery. Early clinical investigations showed during one-lung
ventilation (OLV) there was no difference in oxygenation
when sevoflurane or propofol was administered in patients
undergoing open thoracic surgery.
10,11
This is consistent with our
results of a similar effect on oxygenation by sevoflurane- and
propofol-based anaesthesia in cardiac valve replacement surgery.
However, in another OLV by Cho,
12
desflurane impaired arterial
oxygenation compared with propofol anaesthesia in patients with
thoracoscopic surgery. The discrepancy regarding the effects on
oxygenation by volatile anaesthetics and propofol during OLV
in thoracic surgical patients may be ascribed to different volatile
anaesthetics (sevoflurane vs desflurane) and thoracic surgical
manner (with or without chest opened).
In animal studies, controversy exists regarding the effects of
inhalational anaesthetic agents on oxygenation when compared
to intravenous anaesthetic propofol. Voigtsberger,
7
Schläpfer
13
and Kellner
14
demonstrated that sevoflurane administration led
to a better oxygenation compared to propofol administration
in a rat model of lipopolysaccharide (LPS)-induced mild acute
lung injury (ALI) (mean PaO
2
/FiO
2
~ 400–500 mmHg after two
or three hours of LPS insult). However, in a recent study, the
authors found there was no difference in oxygenation between
isoflurane- and propofol-based anaesthetic regimens in a dog
model of OLV,
15
which is consistent with the finding by Karci
et
al.
16
that sevoflurane and propofol showed comparable effects on
PaO
2
in a rat model of OLV.
In our oleic acid-induced canine severe ALI model (mean
PaO
2
/FiO
2
<
200 mmHg), although the oxygenation was worse
in sevoflurane-sedated dogs compared with propofol-sedated
dogs during a six-hour mechanical ventilation,
5
possibly via
sevoflurane-induced pulmonary vasodilation and its inhibition
of hypoxic pulmonary vasoconstriction (HPV),
17
no difference
was found in oxygenation between seveflurane and propofol at
five and six hours following mechanical ventilation.
5
Different
models and subjects may account for literature discrepancies
in terms of the effects of sevoflurane compared to propofol on
oxygenation in animal experiments.
Our study has limitations. Aone-hour observation period after
CPB with sevoflurane- or propofol-based cardiac anaesthesia
may be too short. Our results reflect only the early time effect
on oxygenation by both anaesthetic regimens during CPB. The
long-term effect of sevoflurane- or propofol-based anaesthesia
on gas exchange deserves further investigation in patients
undergoing cardiac surgery with CPB.
Conclusion
In patients undergoing cardiac valve replacement with CPB, the
changes in PaO
2
/FiO
2
and lung injury were mild, and sevoflurane-
or propofol-based anaesthesia showed a similar effect on
oxygenation, respiratory mechanics and haemodynamics during
the early stage of CPB. Both sevoflurane- and propofol-based
regimens can be used in cardiac anaesthesia.
We acknowledge the grant from National Natural Science Foundation of
China (Grant No. 81872801) to support this study.
PaO
2
/FiO
2
(mmHg)
Fig. 1.
Changes in PaO
2
/FiO
2
at baseline, 15 min after
declamping, and five, 30 and 60 min post-CPB. Red
indicates the sevoflurane group, black indicates the
propofol group (
p
=
0.477 by repeated-measures
ANOVA).



















