
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 3, May/June 2021
AFRICA
145
showed bands of ATP5A and
β
-actin proteins in the ventricles
of different hearts. Semi-quantitatively, there were no significant
differences in the expression of ATP5A among the treatment
groups (Fig. 5B).
There were no significant differences in the plasma Mg
2+
concentration among the groups (concentration of ionised Mg
2+
:
0.89 ± 0.01 mmol/l for control, 0.94 ± 0.05 mmol/l for STZ, 0.85
± 0.04 mmol/l for STZ +Mg
2+
, 0.83 ± 0.01 mmol/l for Mg
2+
;
values are mean ± SEM,
p
> 0.05,
n
= 8 per group).
Discussion
The onset and severity of cardiovascular complications in
poorly controlled diabetes mellitus are time-dependent entities.
In this study, we showed that Mg
2+
treatment induced long-term
improvements in LV contractile function and stabilised heart rate
in chronic diabetic rats.
Our results indicated the presence of diabetes-induced
ventricular systolic dysfunction in chronic diabetes, as was
evidenced by the reduction in LVDP, +dP/dt
max
and the
contractility index in diabetic hearts. These findings are consistent
with the systolic dysfunction reported in chronic type 1 diabetes
patients
18
and in STZ-induced diabetic rats.
19-21
However, the
results are in contrast to the lack of systolic impairment that
we previously observed in the acute diabetes disease model,
14
where only diastolic dysfunction was observed, suggesting a
time-dependent progression of diabetic cardiac complications.
20
In the present study, except for the unaltered time constant
of relaxation (
tau
), diastolic dysfunction was not further
evaluated since the LVEDP had to be pre-set to a fixed value
in order to measure LVDP. Nonetheless, in this study, the
systolic dysfunction in diabetes was reversed by Mg
2+
treatment.
Recently, Mg
2+
was also shown to improve diastolic function and
mitochondrial activity in fat-fed chronic diabetic mice.
22
Given
that diabetic diastolic dysfunction is known to precede systolic
impairment in type 1 diabetic patients
18
and in STZ-induced
diabetic rats,
19,20
and that diastolic dysfunction is a common cause
of systolic heart failure in diabetes,
23
the improvement of systolic
activity by Mg
2+
observed in our study could be secondary to
the diastolic modulation observed in the acute diabetes disease
model.
14
In the present study, there were no detectable cardiac
morphological changes to account for the contractile dysfunction
induced by diabetes. The gross heart weight was unaltered, and
histologically, there was neither a change in cardiomyocyte size
nor interstitial fibrosis. In addition, there was no significant
coronary perivascular fibrosis or cellular infiltrates that would
have been expected to impair coronary perfusion, a finding that
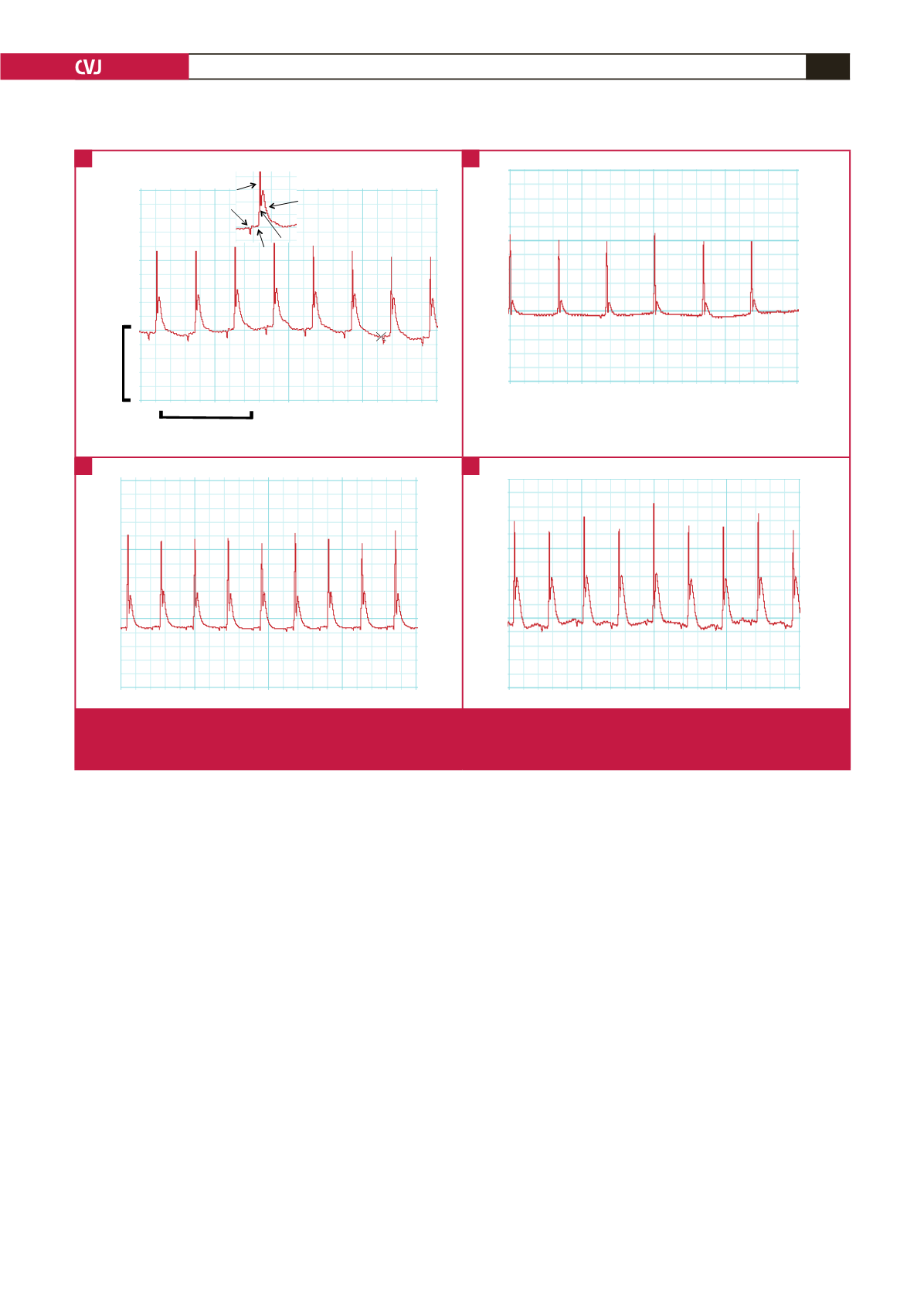
Fig. 3
STZ
Control
STZ+Mg
Mg
(5 mV)
(1 s)
a
b
c
d
P
R
T
Q S
Fig. 3
STZ
Control
STZ+Mg
Mg
(5 mV)
(1 s)
a
b
c
d
P
R
T
Q S
Fig. 3
STZ
Control
STZ+Mg
Mg
(5 mV)
(1 s)
a
b
c
d
P
R
T
Q S
Fig. 3
STZ
Control
STZ+Mg
Mg
(5 mV)
(1 s)
a
b
c
d
P
R
T
Q S
Fig. 3.
Electrocardiographic (ECG) traces. A–D: Representative ECG traces recorded from different isolated hearts during
Langendorff perfusion. Inset in (A) shows labels of the ECG waves. Notice that the S and T waves in the rat heart are
contiguous.
A
C
B
D



















