
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 3, May/June 2021
150
AFRICA
disease, congenital heart disease, previous MV surgery or other
cardiac surgery were excluded. Surgical operative notes were
further scrutinised to determine mitral valve pathology and
document cardiopulmonary bypass times (CPBT).
Two-dimensional directed m-mode and colour Doppler
echocardiography were performed on all patients using a Siemens
Sequoia machine (Acuson, Germany) with a phased-array
transducer and an emission frequency of 3.0MHz with the patient
in the left decubitus position. Images were obtained according
to a standardised protocol. The LV end-systolic (LVESD)
and end-diastolic dimensions (LVEDD), left atrial (LA) size,
pulmonary artery systolic pressures (PASP) and the presence and
severity of tricuspid regurgitation (TR) were measured according
to the American Society of Echocardiography (ASE) chamber
guidelines.
9
EF was assessed using the Simpson’s method.
9
MR was considered to be rheumatic in aetiology when the
morphology of the valve satisfied the proposed World Heart
Federation criteria for the diagnosis of chronic RHD.
10
Clinical
evaluation of the severity of MR in this unit was supported by
colour Doppler estimation of the regurgitant jet into the LA, the
Doppler intensity of the regurgitant envelope, and the LA size
using qualitative and semi-quantitative methods as per ASE and
European Society of Cardiology (ESC) valvular regurgitation
guidelines.
9,11
Calculation of the effective regurgitant orifice using
proximal isovelocity surface area (PISA) was not done because
in most cases the regurgitant flow into the LA was characterised
by an eccentric jet.
The clinical endpoints of this study were cardiovascular
mortality and persistent heart failure postoperatively at the
six-month assessment. Multivariate analysis of pre-operative
EF and other pre-operative echocardiographic parameter/s
(LVEDD, LVESD, LA and PASP) was used to predict post-
operative LV dysfunction. Comparison between the pre- and
postoperative NYHA class was drawn to determine improvement
in functional disability and symptoms.
Statistical analysis
The Statistical Package for Social Sciences (SPSS version 23.0)
(IBM, Los Angeles) was utilised in the analysis of data for the
study. A 95% level of confidence interval (CI) was estimated,
and a global significance level of
ά
= 5% was chosen, to test
for the assumptions of the null hypothesis. Simple descriptive
analysis was used to highlight clinical characteristics and results
are presented as frequencies, means and percentages. Continuous
variables are expressed as means ± standard deviations (SD).
The Student’s
t
-tests and the chi-squared tests were used to
compare continuous and categorical variables, respectively. Paired
samples were used to compare changes in echocardiographic
variables before and after surgery. A
p
-value of < 0.05 suggested
statistically significant findings for the variables being measured.
Comparison between the pre- and postoperative NYHA class
was drawn to determine change in functional disability. Logistic
regression analysis was used to identify pre-operative predictors
of impaired LV function (EF < 50%), and included CPBT as a
potential factor for post-operative LV dysfunction.
Results
During the nine-year period, 788 subjects underwent surgery
for severe MR. Based on the inclusion criteria, a total of 656
patients were excluded, leaving 132 subjects with chronic, severe,
isolated MR for analysis. There were 97 females (73%) and 35
males. Eighty three per cent of patients (
n
= 109) were under the
age of 25 years. In the 75% of subjects who were tested, 8% (
n
=
11) were HIV infected. Other co-morbid conditions were present
in 13% of the sample.
At baseline, 66% (
n
= 87) of patients were in NYHA
functional class III–IV (NYHA III, 30%, NYHA IV, 36%).
Heart failure with fluid overload was a common mode of
presentation and was present in 38% (
n
= 50) of subjects, and
14% (
n
= 19) had atrial fibrillation prior to surgical intervention
(Table 1). Medication prescribed to the patients in the study
included diuretics (92%), angiotensin converting enzyme (ACE)
inhibitors (95%),
β
-blockers (8%), calcium channel blockers
(2%), digoxin (21%) and penicillin (72%).
For the entire group, the median EF was 63% (IQR 58–70%),
mean LVEDD 60.7 ± 7.9 mm, LVESD 39.9 ± 7.2 mm, and
LA size 61.2 ± 12.6 mm. The median PASP was 59.5 mmHg
(IQR 45–80 mmHg). Pre-operatively, 72% (
n
= 95) had an EF
> 60% (median EF 65%, IQR 62–70%), 5% (
n
= 7) had an EF
between 40 and 49% (median EF 42%, IQR 40–45%) and 23%
(
n
= 30) had an EF between 50 and 59% (median EF 56%, IQR
55–57%). The LVEDD and LVESD were significantly higher in
both groups with EF < 60% compared to EF > 60% (
p
< 0.001).
The LA was grossly enlarged (over 55 mm) across all three EF
groups and the PASP was similarly elevated in all three groups.
Moderate to severe TR was present in all seven subjects in the
EF 40–49% group, 62% of those in the EF 50–59% group and in
58% of those with EF > 60% (Table 2).
The patients’ operative notes were studied to determine the
macroscopic pathology of mitral valve disease as described by
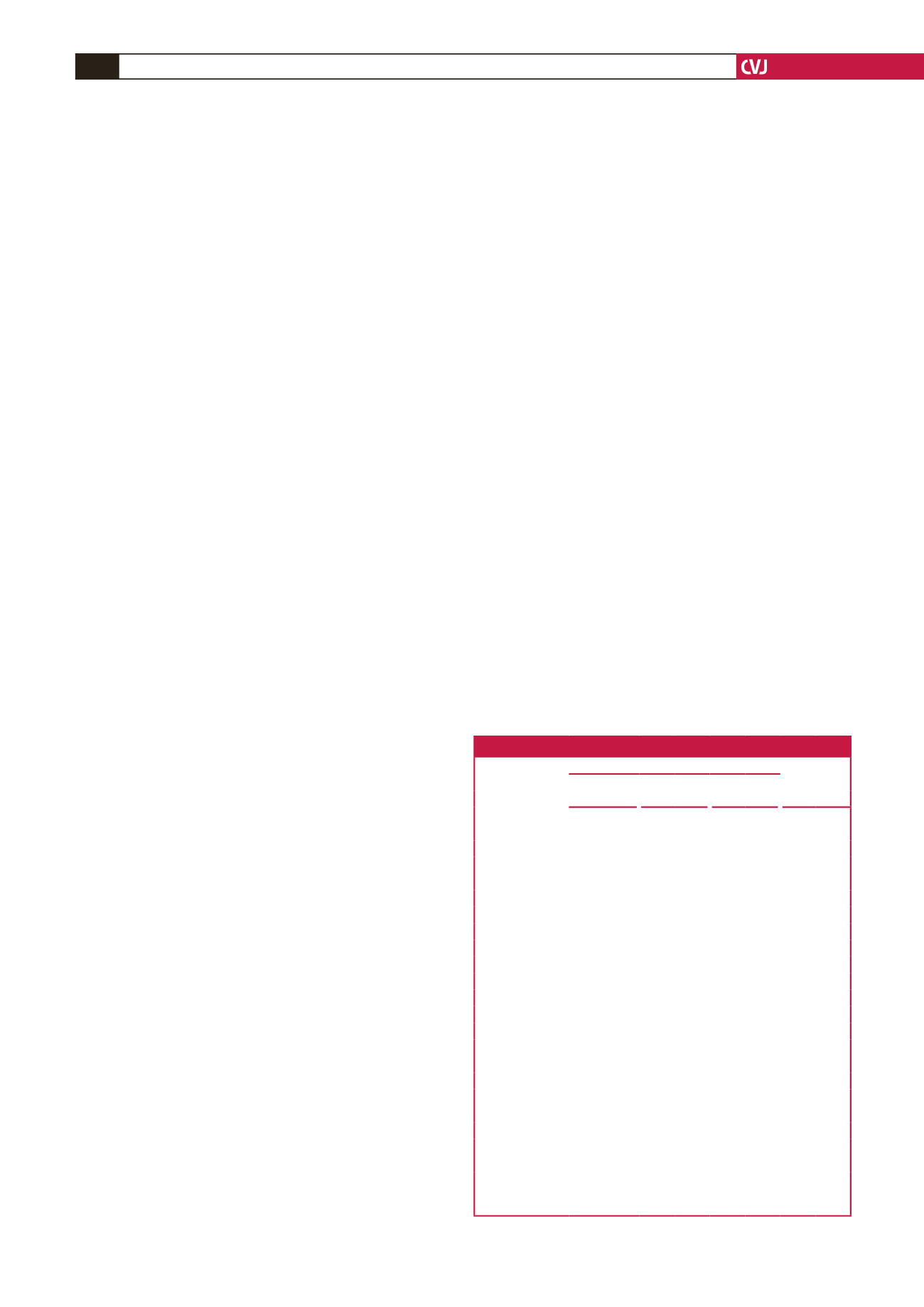
Table 1. Baseline demographic and clinical data
EF group
Total
(n = 132)
40–49%
(n = 7)
50–59%
(n = 30)
> 60%
(n = 95)
Age group (years)
n
% n
% n
% n
%
< 12
1 14
3 10 39 41 43 33
12–25
4 57 20 67 42 44 66 50
> 25
2 29
7 23 14 15 23 17
Gender
Male
2 29
7 23 26 27 35 27
Female
5 71 23 77 69 73 97 73
HIV
Negative
4 57 23 77 61 64 88 67
Positive
1 14
3 10 7
7 11
8
Not known
2 29
4 13 27 28 33 25
NYHA class
I
0
0
1 3
9
9 10
8
II
1 14
9 30 25 26 35 27
III
2 29
8 27 29 31 39 30
IV
4 57 12 40 32 34 48 36
Heart failure
Present
5 71 13 43 32 34 50 38
Absent
2 29 17 57 63 66 82 62
AF
Present
1 14
4 13 14 15 19 14
Absent
6 86 26 87 81 85 113 86
AF, atrial fibrillation; EF, ejection fraction; NYHA, New York Heart Associa-
tion. Only 23 subjects were over the age of 25 years. The majority was HIV
negative.



















