
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 32, No 3, May/June 2021
AFRICA
147
was also consistent with the lack of change in coronary flow rate
observed in this study.
These findings are in agreement with those in other studies
on chronic STZ-induced diabetic rats in which the cardiac
dysfunction was not accompanied by histological evidence of
cardiac cellular hypertrophy or fibrosis.
20
In contrast, other
studies in chronic STZ-induced diabetic rats showed that there
was cardiac dysfunction together with histological evidence of
cardiomyocyte hypertrophy and fibrosis.
24
These histological
differences are likely to be related to the duration of diabetes,
given that in diabetic patients, the deposition of collagen in
cardiac tissue only becomes more prominent in the later stages of
heart failure when there is a low ejection fraction.
25
In our study, there were no significant cardiac histological
changes to account for the effect of Mg
2+
. Taken together, the
lack of histological alterations in our study supports the concept
that the nature of diabetic ventricular dysfunction and the effect
of Mg
2+
were functional, rather than structural.
The STZ-induced decrease in heart rate observed in the
present study and its prevention by Mg
2+
were consistent with
our previous findings in the acute-diabetes model where the
relative bradycardia was also observed
in vivo
.
14
The bradycardia
in STZ-induced diabetic rats has also been reported in other
studies,
20,26
and has been attributed to cardiac autonomic synaptic
degradation,
26
but the basis of the bradycardia in our study
remains unclear. In this study, the bradycardia seemed to
be unrelated to the modulation of cardiac electrical activity
since there were no significant changes in ECG waves. The
prolongation of the QT interval in diabetes was probably related
to changes in heart rate because the QT interval, corrected for
the heart rate (QTc), was not significantly different among the
treatment groups. Taken together, the occurrence of bradycardia
both
in vivo
and
ex vivo
and its prevention by Mg
2+
suggest that
these effects were intrinsic to the heart.
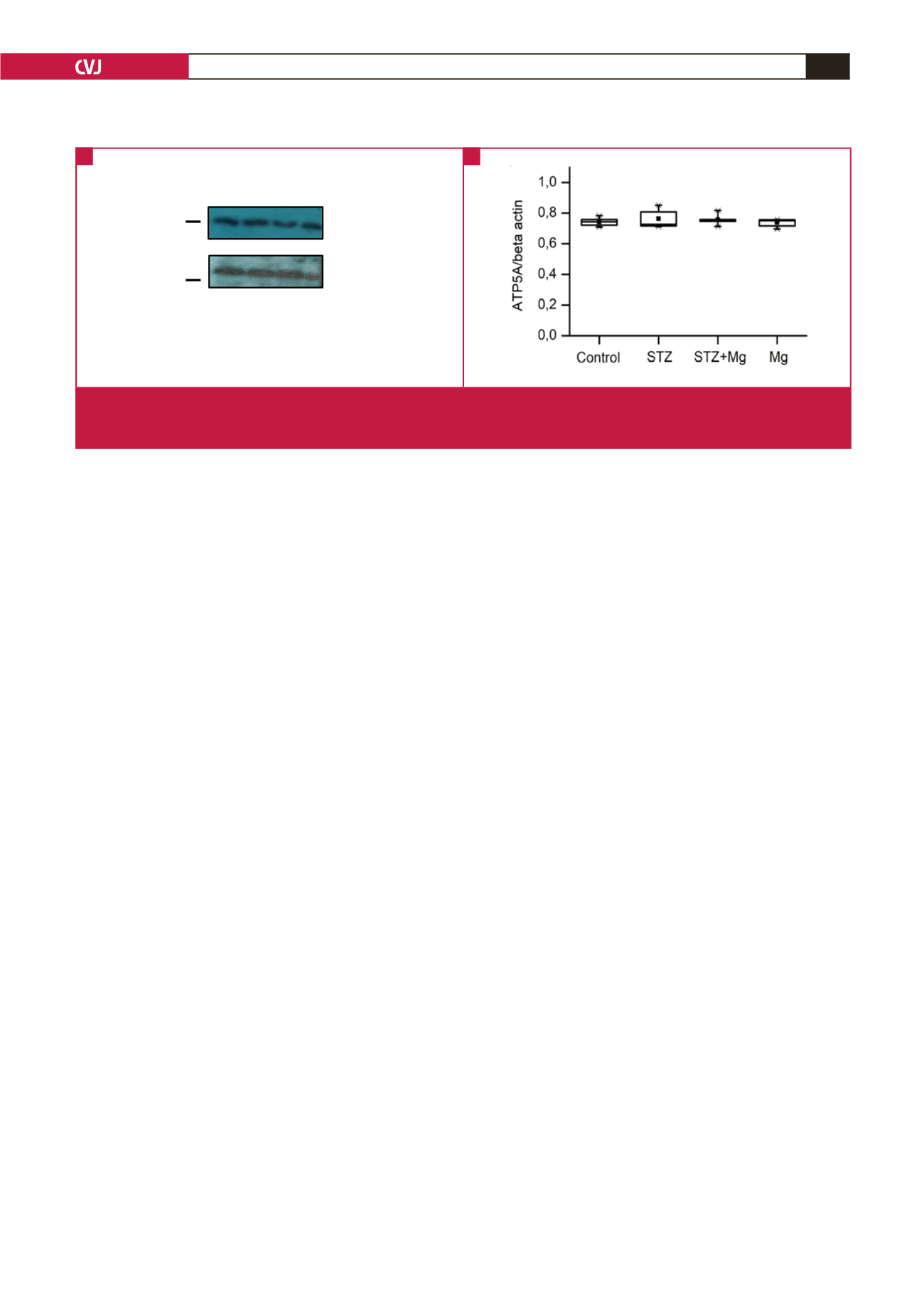
Despite the improvements in cardiac function by Mg
2+
,
there were no significant differences in the cardiac expression
of ATP5A, a cardiac biomarker that could have accounted for
the Mg
2+
effects at a molecular level. Mg
2+
is a key co-factor of
several co-enzymes that may alter the cardiac metabolic status,
it also contributes to cellular energetics via its coupling with
ATP to form MgATP,
13
and it may therefore alter mitochondrial
function. However, in our study, there were no changes in
the metabolic indices, as was indicated by the mitochondrial
metabolic component ATP5A. Therefore, further molecular
studies such as those evaluating aspects of mitochondrial fusion/
fission are required to elucidate the role of Mg
2+
at the cardiac
cellular level.
Limitations of this study include the use of an artificial,
STZ-induced diabetic model, in which the Mg
2+
effects may
not be readily translatable to the natural disease. However, the
STZ-induced diabetic rat model is known to mimic diabetic
complications in humans.
21
We also previously showed the value of
this disease model in that, apart frommimicking type 1 diabetes, it
also exhibited features of type 2 diabetes, such as dyslipidaemia.
14
Also, the clinical relevance of the Mg
2+
dose used in this study
remains unclear, given that that the dose (270 mg/kg) is higher
than that used via the oral route in human supplementation,
and is only comparable to the loading intravenous/intramuscular
dose used in eclampsia (~ 230 mg/kg).
27
Nonetheless, the peak
increases at 3.5 hours of ~ 0.7 mmol/l, achievable under our
experimental conditions,
15
are still within the therapeutic ranges
of other clinical conditions.
27
Finally, since the experiments were
performed at cardiac tissue level, the presence of an intracellular
Mg
2+
deficit cannot be excluded, and therefore requires further
investigations at a cellular level.
Conclusion
The results of this study show that Mg
2+
improved cardiac
contractile function and stabilised heart rate in the STZ-induced
chronic diabetes rat model, without preventing metabolic
derangements such as hyperglycaemia. The mechanisms under-
lying the attenuation of cardiac dysfunction in chronic diabe-
tes mellitus by Mg
2+
were unrelated to electrocardiographi-
cally or histologically detectable changes, but the exact pathways
involved require further investigation.
The study was supported by the South African Medical Research Council
(MRC, Grant No 29841) and by the National Research Foundation (NRF)
of South Africa (Grant No 91514).
References
1.
Beckman JA, Creager MA. Vascular complications of diabetes.
Circ Res
Fig. 5
a
β
-actin
ATP5A
MW
(
kDa
)
53
38
Control
STZ
STZ+Mg
Mg
Fig. 5
a
β
-actin
ATP5A
MW
(
kDa
)
53
38
Control
STZ
STZ+Mg
Mg
Fig. 5.
Western blot analysis of mitochondrial ATP5A protein. A: Representative Western blot film images of ATP5A and the corre-
sponding
β
-actin in ventricular tissue of different hearts. B: Summary data of the fold-expression of ATP5A, normalised to
that of
β
-actin. Data are shown as box plots and the mean (
■
);
n
= 3 per group.
A
B
-



















