
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
AFRICA
101
sense to patients, and it is incumbent on the clinician to take
the time to allay fears, ensuring good and clear communication
during counselling.
‘Safe’ is a relative term but one that physicians should not be
afraid to use. When a radiographic study is needed for appropriate
management of a pregnant patient, the ACR recommends that
‘health care workers should tell patients that X-rays are safe and
provide patients with a clear explanation of the benefits of X-ray
examinations.’
74
One tool that physicians may consider using
to reassure patients is Table 3, which compares the dosage of
radiation provided by various common diagnostic studies with
the accepted limit of 5 rad (50 mSv). A patient’s particular study
could also be plotted on this graph, showing the clear margin of
safety that exists for all single diagnostic studies.
Conclusion
Pregnant women with known or suspected CVD often require
cardiovascular imaging. The accepted maximum limit of ionising
radiation exposure to the foetus during pregnancy is a cumulative
dose of 5 rad (50 mSv or 50 mGy). Concerns related to imaging
modalities that involve ionising radiation include teratogenesis,
mutagenesis and childhood malignancy. Importantly, no single
imaging study approaches this cautionary dose of 5 rad (Table
4). Elective studies may be deferred until the pregnancy is over
or the gestational period is beyond 20 weeks, and there are
several strategies that may be employed to minimise radiation
to the foetus (Table 3). Echocardiography and CMR appear
to be completely safe in pregnancy and are not associated with
any adverse foetal effects, provided there are no general contra-
indications to MR imaging. Current evidence suggests that a
single cardiovascular radiological study during pregnancy is safe
and should be undertaken at all times when clinically justified.
As a general guide, centres where medical imaging is
performed should have signs to remind mothers to notify the
staff if they may be pregnant. The potential risks of each
imaging modality must be discussed with the mother before
she undergoes such imaging. Pregnant women must be made
to understand that exposure from a single diagnostic procedure
does not result in harmful foetal effects. Specifically, exposure
to less than 5 rad has not been associated with an increase in
foetal anomalies or pregnancy loss. Therefore concerns about
possible effects of high-dose ionising radiation exposure should
not prevent medically indicated diagnostic X-ray procedures
from being performed on pregnant women. Consultation with
an expert in dosimetry calculation may be helpful in calculating
estimated foetal dose when multiple diagnostic X-ray procedures
are performed in pregnancy.
In general, the radiation safety principle, ALARA (as low
as reasonably achievable), minimising radiation and release
of radioactive materials should be employed at all times. In
addition, the use of iodine-based contrast agents for X-ray,
fluoroscopy and CT scanning, and the use of gadolinium-based
contrast agents for CMR are safe in pregnancy and should be
used when the potential benefit justifies the potential risk to
the foetus. However, the use of radioactive isotopes of iodine is
contra-indicated for therapeutic use during pregnancy.
Dr Ntusi acknowledges support from the National Research Foundation and
Medical Research Council of South Africa.
References
1.
ACOG Committee on Obstetric Practice. ACOG Committee Opinion.
Number 299, September 2004 (replaces No. 158, September 1995).
Guidelines for diagnostic imaging during pregnancy.
Obstet Gynecol
2004;
104
(3): 647–651.
2.
Hall EJ. Scientific view of low-level radiation risks.
Radiographics
1991;
11
(3): 509–518.
3.
Brent RL. Utilization of developmental basic science principles in the
evaluation of reproductive risks from pre- and postconception environ-
mental radiation exposure.
Teratology
1999;
59
: 182-204.
4.
International Commission on Radiological Protection. Pregnancy
and medical radiation.
Annals of the International Commission on
Radiological Protection.
Oxford: Pergamon Press, 2000, Publication 84.
5.
Gray JE. Safety (risk) of diagnostic radiology exposures. In:
American
College of Radiology. Radiation Risk: a Primer
. Reston (VA): ACR’
1996: 15–17.
6.
Brent RL. The effect of embryonic and fetal exposure to X-ray, micro-
waves, and ultrasound: counseling the pregnant and nonpregnant
patient about these risks.
Semin Oncol
1989;
16
: 347–68.
7.
Parry RA, Glaze SA, Archer BR. The AAPM/RSNA physics tutorial
for residents. Typical patient radiation doses in diagnostic radiology.
Radiographics
1999;
19
: 1289–1302.
8.
Wieseler KM, Bhargava P, Kanal KM, Vaidya S, Stewart BK, Dighe
MK. Imaging in pregnant patients: examination appropriateness.
Radiographics
2010;
30
(5): 1215–1233.
9.
Streffer C, Shore R, Konermann G,
et al
. Biological effects after
prenatal irradiation (embryo and fetus). A report of the International
Commission on Radiological Protection.
Ann Int Comm Radiol Protect
2003;
33
(1–2): 5–206.
10. McCollough CH, Shueuler BA, Atwell TD, Braun NN, Renger DM,
Brown DL,
et al
. Radiation exposure and pregnancy: should we be
concerned?
Radiographics
2007;
27
: 909–918.
11. Toppenberg KS, Hill DA, Miller DP. Safety of radiographic imaging
during pregnancy.
Am Fam Physician
1999;
59
(7): 1813–1818.
12. Loganovsky K. Do low doses of ionising radiation affect the human
brain?
Data Science J
2009;
8
: 13–35.
13. Wagner LK, Lester RG, Saldana LR.
Exposure of the Pregnant Patient
to Diagnostic Radiations: a Guide to Medical Management.
Madison,
USA: Medical Physics Publishing, 1997.
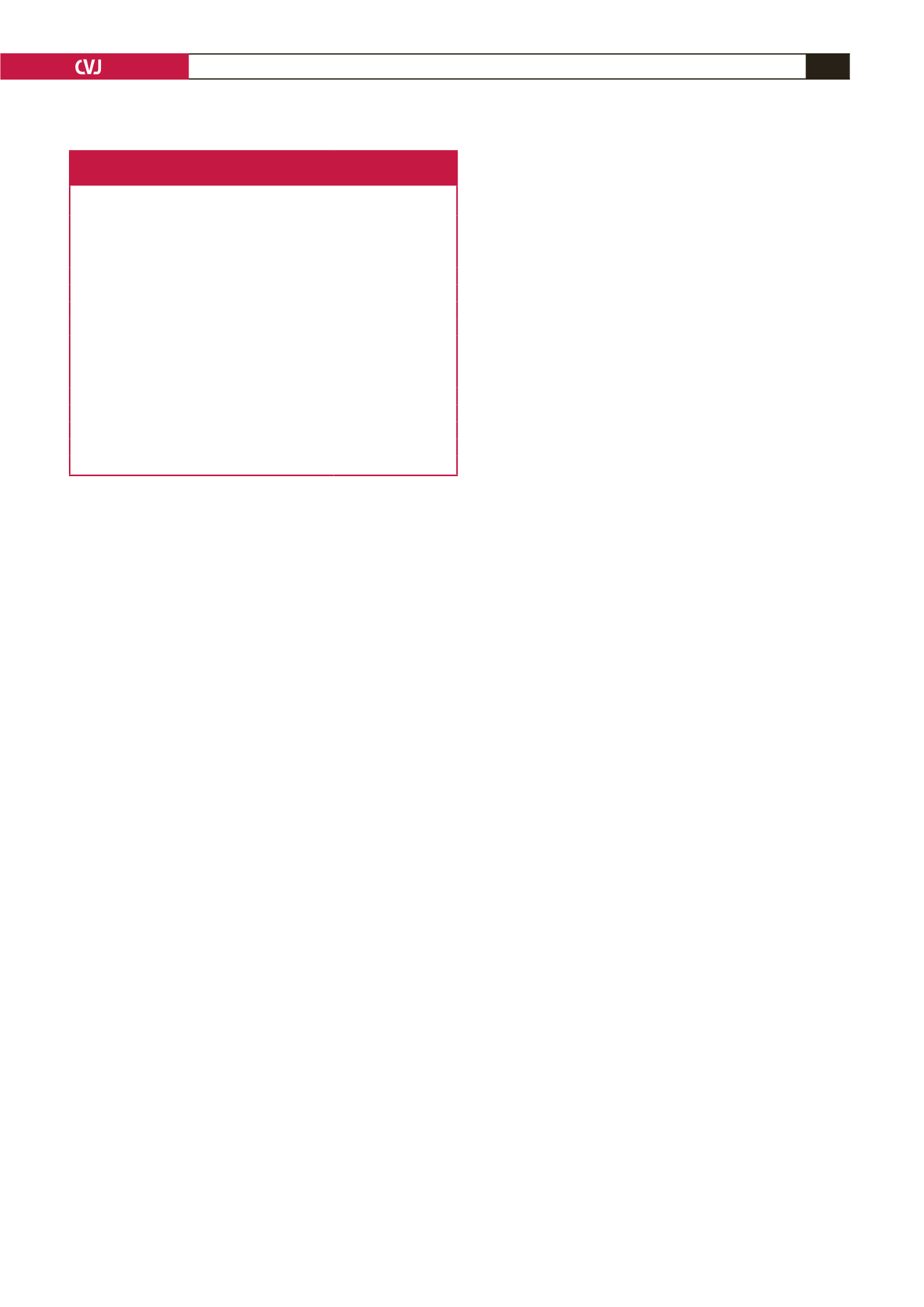
Table 4. Doses to the foetus from radiological and
nuclear medicine examinations
Examination
Estimated foetal dose
(mGy)
Chest radiograph
< 0.0001
Pulmonary CTA
0.01–0.66
CCTA (prospective gating)
1.0
CCTA (retrospective gating)
3.0
Abdominopelvic CTA
6.7–56.0
Direct fluoroscopy (groin to heart catheter passage) 0.094–0.244 mGy/min
Coronary angiography
0.074
Electrophysiological procedures
0.0023–0.012 mGy/min
Lung perfusion
0.6
Lung ventilation
0.005–0.09
Myocardial perfusion
5.3–17
Gated blood pool
6.0
PET viability
6.3–8.1
PET perfusion
2.0
Maximum recommended dose
5 rad or 50 mGy

















