
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
AFRICA
97
microcephaly.
15
A linear, dose-related association between severe
mental retardation and radiation was also found, with the
important caveat that most cases followed exposure during weeks
eight to 15 of gestation.
16,17
Radiation-induced malignancy
Exposure to as little as 1 or 2 rad has been associated with
an increase in childhood malignancies, especially leukaemia,
occurring in a stochastic fashion.
13
For example, the background
rate of leukaemia in children is about 3.6 per 10 000.
18
Exposure
to 1 or 2 rad increases this rate to five per 10 000.
19
While these
doses do fall within the range of some radiographic studies, the
absolute increase of risk (~ 1 in 10 000) is very small.
20
Therefore,
physicians should carefully weigh the risks and benefits of any
radiographic study and include the mother in the decision-
making process whenever possible.
Radiation-induced mutagenesis
Radiation can cause germ-line mutations, potentially affecting
future generations. Although radiation is commonly believed to
create bizarre new mutations, data show that it usually merely
increases the frequency of mutations occurring naturally in
the general population.
21
The dosage required to double this
baseline mutation rate is between 50 and 100 rad, far more
than the radiation doses occurring in common cardiovascular
radiographic studies.
22
The most important factor for physicians to remember is
that the currently accepted maximum limit of ionising radiation
exposure to the foetus during pregnancy is a cumulative dose of
5 rad (50 mSv or 50 mGy).
3,10,20,23
Non-ionising radiation and pregnancy
The reproductive risk of non-ionising radiation, which includes
electromagnetic fields from computers, microwave ovens,
microwave communication systems, cellular phones, power lines,
household appliances, heating pads and warming blankets,
airport metal screening devices and diagnostic ultrasound has
been studied extensively. Two national committees of scientists
in the US evaluated the risk from these non-ionising radiation
sources. The first report was published in 1993 from the Oak
Ridge Associated University panel
24
created by the White House,
while the second was the product of the committee of the
National Academy of Sciences.
25
Both of these groups concluded
that the reproductive risk of non-ionising radiation is minimal,
if even existent.
24,25
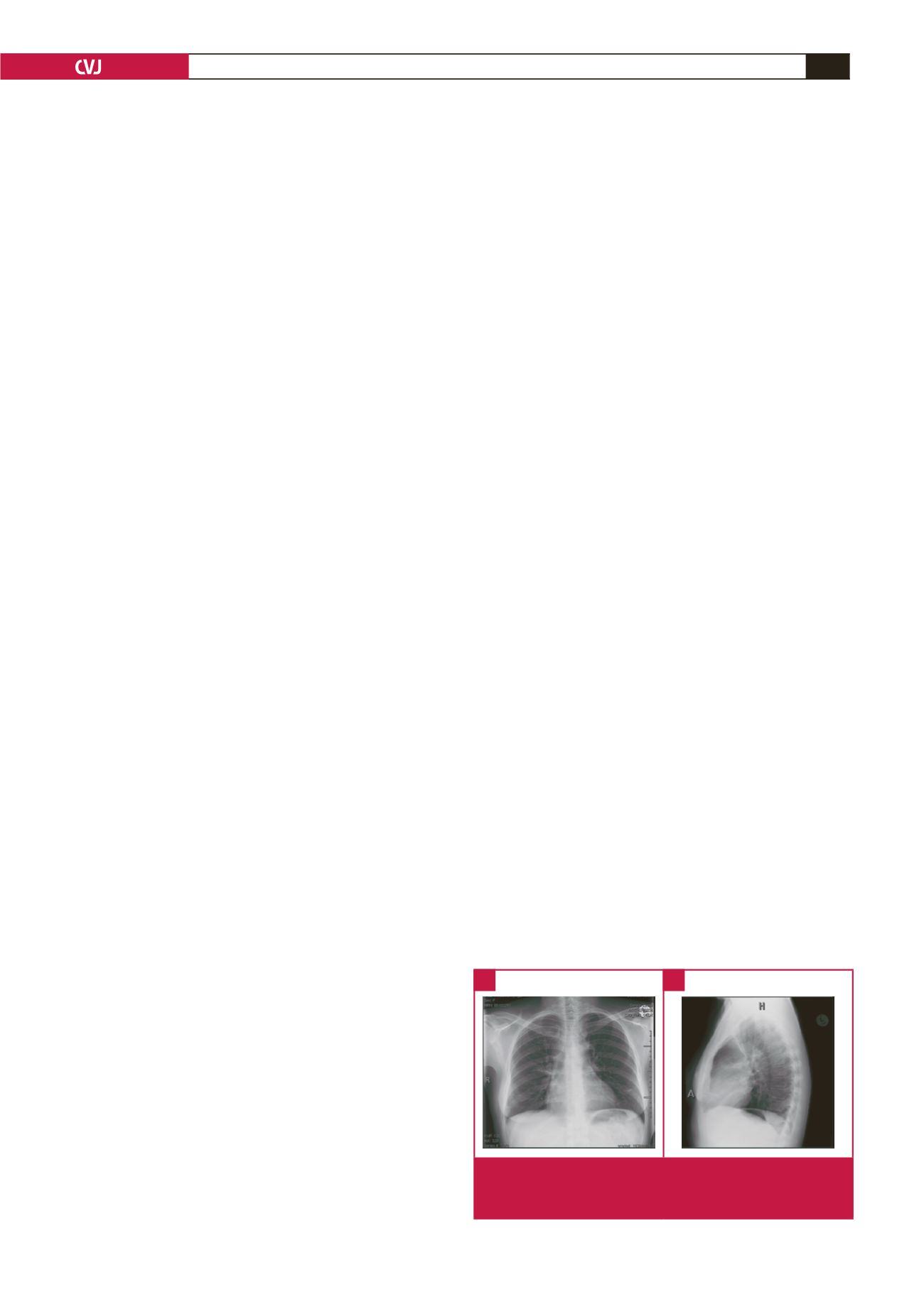
Chest radiography
The chest X-ray is the most commonly performed diagnostic
cardiovascular radiographic examination, and is able to produce
accurate images of the heart, lungs, airways, blood vessels and
the bones of the spine and chest. The chest X-ray utilises small
amounts of radiation (0.00002 to 0.00007 rad)
4,9
when a focused
beam of radiation is passed through the body, resulting in a
black-and-white image recorded on special film or a computer.
X-rays are able to differentiate tissues in the body because
of varying densities (each tissue allows a different amount of
radiation to pass through and expose the X-ray-sensitive film).
26
Dense bone absorbs much of the radiation while soft tissue,
such as heart muscle, allows more of the X-rays to pass through.
Consequently bones appear white on the X-ray, soft tissue shows
up in shades of grey and air appears black.
Medically indicated diagnostic chest radiographic studies
can be safely performed in pregnancy (Fig. 1), provided the
equipment works properly and the abdomen of the patient is
adequately shielded. The risk of not making the diagnosis often
far surpasses the risk of radiation in such instances.
27
Fluoroscopy and invasive angiography
Fluoroscopy is a type of medical imaging that shows a
continuous X-ray image on a monitor, much like an X-ray
movie. Fluoroscopy is routinely used to screen suspected stuck
prosthetic valves and for percutaneous transvenous mitral
commissurotomy (PTMC) in those with symptomatic mitral
stenosis in pregnancy. Furthermore, fluoroscopy is the basis
for imaging during invasive angiographic procedures (including
coronary angiography and haemodynamic studies). There
are many situations where the benefit of performing these
procedures is much greater than any small possible harm that
might arise from radiation exposure.
20
For a typical fluoroscopic
study, the amount of radiation occurring is in the range of 0.001
to 0.05 rad; dosage depends on duration of fluoroscopic time.
28
As always with any medical exposure, each particular
procedure must be clinically justified, including taking into
account when the procedure needs to occur and the anticipated
radiation dose to the foetus. Once justified, due diligence is
taken to optimise when and how the procedure is performed
to minimise radiation exposure to the foetus, consistent with
achieving the desired clinical outcome. The radiation exposure to
the foetus predominantly arises from scattered radiation within
the patient.
20,29
Some of the main methods for minimising the dose to the
foetus include: (1) restricting the X-ray beam size to as small
as is necessary; (2) choosing the direction of the primary
beam so that it is as far away from the foetus as possible; (3)
ensuring that the overall exposure time is as short as possible; (4)
selecting appropriate exposure factors; (5) calculating the dose
by a knowledgeable medical physicist, if there is concern; and (6)
using a lead apron on the table to shield any primary beam from
the X-ray tube reaching the foetus (Table 3).
Fig. 1.
Chest radiography of a pregnant woman with peripar-
tum cardiomyopathy. (A) posterior lateral projection, (B)
lateral projection.
A
B

















