
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
96
AFRICA
Possible deleterious effects of ionising radiation include (1)
genetic consequences, the risks of which can be assessed only
from animal studies; (2) carcinogenesis, which can be assessed
from survivors of nuclear bombings and patients exposed for
medical reasons; and (3) teratogenic effects on the developing
embryo or foetus.
2
Most cardiovascular diagnostic procedures
expose the embryo and foetus to less than 50 mSv,
5
which
does not increase reproductive risks (either birth defects or
miscarriage).
6
The reported dose of radiation with consequent increased
incidence of birth defects or miscarriage is above 200 mSv.
7
Termination of pregnancy on the grounds of ionising radiation
exposure is not recommended unless there is sufficient
documentation that the estimated foetal dose exceeds 15 rad
(150 mSv).
8
An important determinant of the consequence of radiation
exposure in pregnancy is the stage in which the radiation
exposure occurs.
1,9
In the first two weeks following conception
or the second two weeks from the last menstrual period, the
developing embryo is resistant to the malforming effects of
X-rays. However, the developing embryo is sensitive to the
lethal effects of X-rays, although doses much higher than
5 rad (50 mSv) are necessary to cause a miscarriage.
10
From the
third to the eighth week of pregnancy, in the period of early
embryonic development, the embryo is hardly affected, in terms
of birth defects, pregnancy loss, or growth retardation, unless the
exposure is substantially above 200 mSv.
11
From the eighth to the
15th week of pregnancy, the embryo or foetus is sensitive to the
effects of radiation, particularly on the central nervous system
(CNS). However, for the development of microcephaly and other
CNS malformations, the radiation exposure has to be sufficiently
high. The threshold for an observed effect on intelligence
quotient is estimated to be greater than 30 rad (300 mSv).
12
Cardiovascular diagnostic studies do not reach these levels
and, therefore, these effects are rarely of concern for patients.
The most sensitive period for CNS teratogenesis is between eight
and 15 weeks of gestation, therefore non-urgent radiological
testing should be avoided during this time. Rare consequences
of prenatal radiation exposure include a slight increase in the
incidence of childhood leukaemia and, possibly, a small change
in the frequency of genetic mutations.
13
Such exposure is not an
indication for pregnancy termination, however.
Appropriate counselling of patients before radiological
studies are performed is critical. After 20 weeks of gestation,
the foetus is fully developed and it again becomes resistant to
the effects of radiation exposure. At this late stage, there is no
evidence of increased risk of birth defects or miscarriage from
radiological diagnostic studies.
14
Deleterious effects of ionising radiation
Radiation-induced teratogenesis
CNS malformations, in particular microcephaly and mental
retardation, are the most commonly seen non-stochastic
complications following high-dose radiation exposure.
Following Hiroshima, many Japanese bomb victims who were
exposed
in utero
to doses greater than 10 to 150 rad developed
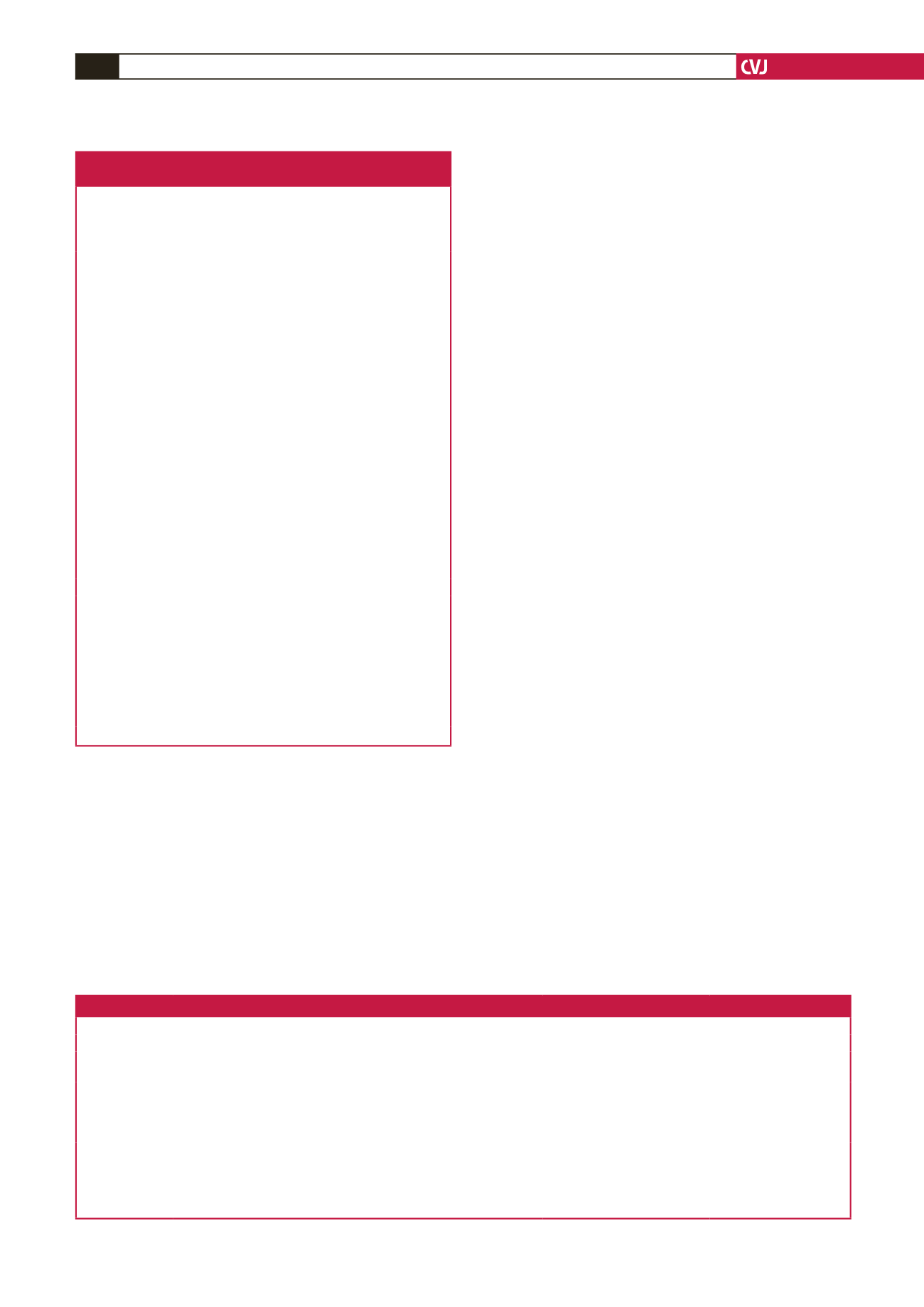
Table 1. Rationale for use and indications for
imaging of CVD in pregnancy
Evaluation of biventricular structure, size and function
Evaluation of native and prosthetic valve disease
Evaluation of pregnancy-induced hypertension and hypertensive heart
failure of pregnancy
Evaluation of congenital heart disease
Evaluation of myocarditis
Evaluation of specific cardiomyopathies
• Dilated cardiomyopathy
• Peripartum cardiomyopathy
• Hypertrophic cardiomyopathy
• Arrhythmogenic right ventricular cardiomyopathy
• Iron-overload cardiomyopathy
• Restrictive cardiomyopathy
• Myocardial infiltration (e.g. sarcoidosis)
• Left ventricular non-compaction
• Systemic rheumatic diseases (e.g. rheumatoid arthritis, systemic lupus
erythematosus, systemic sclerosis)
• Other less-common diseases (e.g. Chagas disease, Churg-Strauss
syndrome)
Evaluation of pericardial disease
• Pericarditis
• Pericardial effusions
• Pericardial tumours
• Pericardial effusive-constrictive syndrome
• Pericardial constriction
Evaluation of great vessels and pulmonary veins
Evaluation of cardiac masses (differentiation of tumour from thrombus)
Evaluation of infective endocarditis
Evaluation of ischaemic heart disease
• Diagnosis of myocardial infarction and its sequelae
• Assessment of myocardial viability
• Assessment for inducible ischaemia
• Coronary imaging
• Assessment of suspected coronary artery fistula
• Assessment of suspected anomalous coronary origins
Differentiation of ischaemic versus non-ischaemic cardiomyopathy
Evaluation of mechanical dyssynchrony
Evaluation of unexplained heart failure or stroke
Table 2. Measures of ionising radiation
Measure
Definition
Conventional units
SI units
Exposure
Number of ions produced by X-rays per kg of air
Roentgen (R)
Coulombs/kg (C/kg)
Absorbed dose Amount of energy deposited per kg of tissue
Radiation absorbed dose (rad) Gray (Gy)
1 Gy = 100 rad
KERMA
Kinetic energy released per unit mass
Radiation-absorbed dose (rad) Gray (Gy)
1 Gy = 100 rad
Dose equivalent A measure of radiation-specific biological damage in humans
Roentgen equivalents man (rem) Sievert (Sv)
1 Sv = 100 rem
Relative effective
dose
Amount of energy deposited per kg of tissue normalised for biological
effectiveness
Roentgen equivalents man (rem)
(1 rem = 1 rad for X-rays)
Sievert (Sv)
1 Sv = 100 rem
(1 Sv = 100 rad for X-rays)
Activity
Amount of radioactivity expressed as the nuclear transformation rate
Curie (Ci)
Bequerel (Bq)
1 Ci = 3.7 × 10
10
Bq

















