
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 2, March/April 2016
AFRICA
99
shielding, lowering the peak kilovoltage or lowering the tube
current.
43
In general, lower-dose protocols result in images with
poor resolution and greater noise, therefore reductions must
consider image quality and diagnostic confidence.
44
CTPA remains the imaging modality of choice for diagnosis
of pulmonary embolism in pregnancy and is preferred for its
general superiority over ventilation-perfusion scintigraphy.
45
Ventilation-perfusion scintigraphy may be indeterminate in up
to 25% of patients imaged in pregnancy.
46
In addition, the foetal
radiation dose from CTPA is substantially less than that from
ventilation-perfusion scintigraphy in all trimesters, even if half-
dose perfusion-only scintigraphy is used.
47,48
Cardiovascular magnetic resonance
CMR is a remarkably powerful imaging modality, free of
ionising radiation, with high spatial and temporal resolution,
performed via excitation of hydrogen protons within a powerful
magnetic field.
49
The strong magnetic field aligns the nuclear
magnetisation spin of the hydrogen protons, which are then
excited by radiofrequency (RF) pulses (pulse sequences). After
the RF pulses are switched off, the protons give off energy
as they precess back to their equilibrium magnetisation; this
dissipated energy is detected by the MR receiver coils. Fourier
transformation is then used to convert frequencies into images.
The signal from a given tissue (e.g. heart muscle) is determined
by the proton density (PD) and by two specific relaxation
parameters: longitudinal relaxation time (T1) and transverse
relaxation time (T2).
49
PD, T1 and T2 vary substantially for
different tissues, and may vary substantially within the same
tissue from health to disease; these differences are used to
generate contrast in MR images.
50
To prevent artifacts from
cardiac motion, CMR images are generated with fast sequences
gated to the Rwave of the electrocardiogram. Respiratory motion
may be eliminated by acquiring CMR images in end-expiratory
breath-hold.
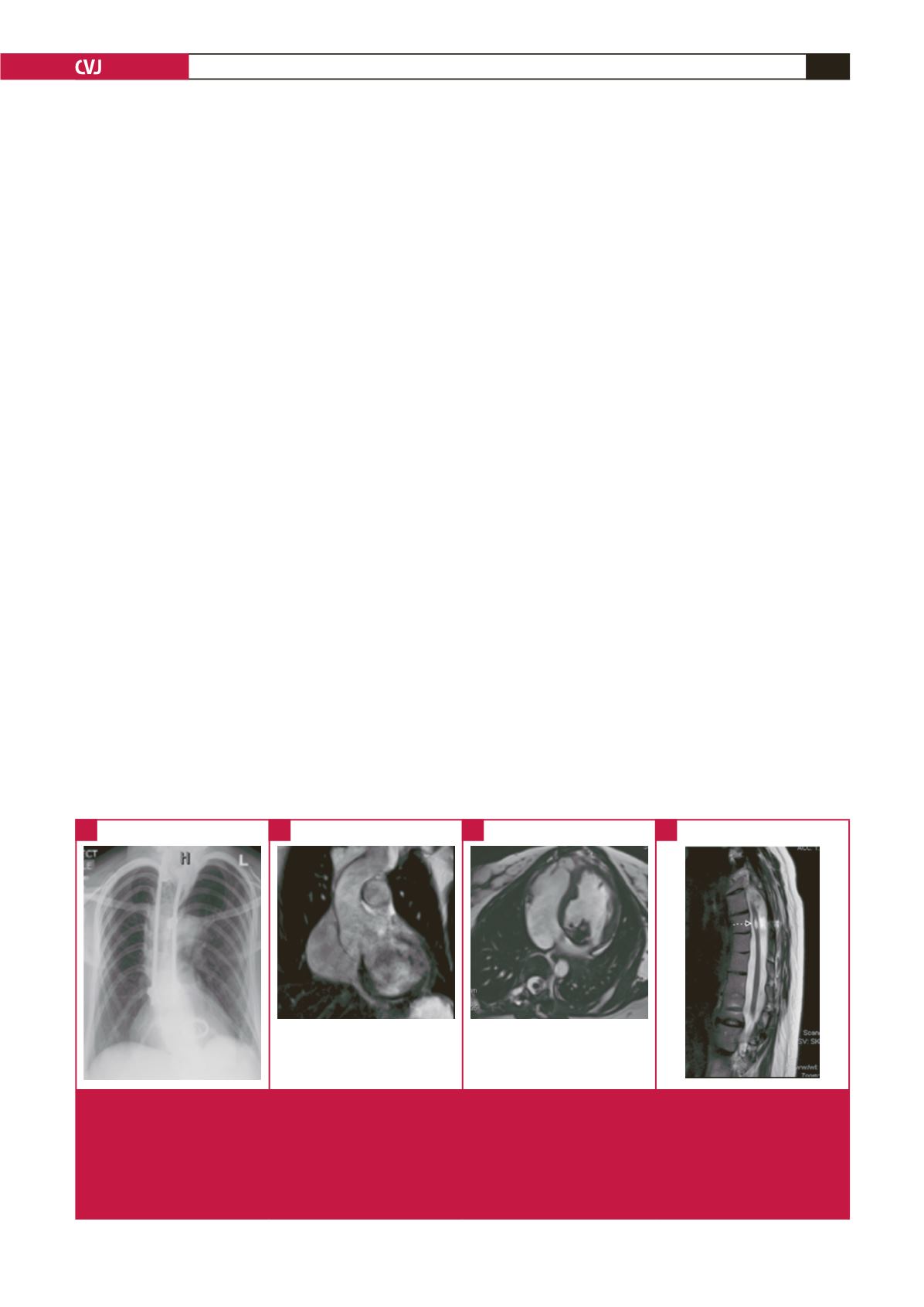
MR has been used to evaluate obstetric, placental and foetal
abnormalities in pregnant patients for more than 25 years. MR
imaging is recognised as a beneficial diagnostic tool and is utilised
routinely to assess multiple conditions that affect the pregnant
patient (Fig. 3) as well as the foetus. To date, there has been a
paucity of systematic studies directed towards determining the
relative safety of using MR procedures in pregnant patients.
51
There has been no evidence of harm from the use of CMR and
other forms of MR imaging in pregnancy.
51
Safety concerns include possible bio-effects of the static
magnetic field of the MR system, risks associated with exposure
to the gradient magnetic fields, the potential adverse effects of
RF energy, possible adverse effects related to heating and to
the combination of these three electromagnetic fields, possible
acoustic injury from the vibration and noise in the scanner, and
possible toxicity from gadolinium-based contrast agents used in
patients with renal dysfunction.
52
MR environment-related risks
are difficult to assess for pregnant patients due to the number of
possible permutations of the various factors that are present in
this setting (e.g. differences in field strengths, pulse sequences,
exposure times).
However, several experimental and clinical investigations of
the effects of MR in pregnancy showed no evidence of injury
or harm to the foetus or the mother.
53,54
Even the few human
studies performed in pregnant human subjects exposed to MR
imaging or the MR environment have not reported adverse
outcomes for the subjects.
55,56
In recent times, there has been
increasing concern that acoustic noise associated with MR may
impact on the foetus; however this remains unproven in recent
large studies.
57
In summary, CMR up to 3T appears to be safe in all stages
of pregnancy.
58
Higher field strengths have not been evaluated
in the setting of pregnancy. CMR, where available, together
with echocardiography, remains preferable to any studies using
ionising radiation for cardiovascular imaging in pregnancy, in
particular during the first trimester. Despite the lack of harm
Fig. 3.
CMR imaging in a pregnant woman with Marfan syndrome with previous spinal surgery and a prosthetic mitral valve (for
severe mitral regurgitation). (A) anterior–posterior projection of chest radiograph showing scoliosis, spinal rods and pros-
thetic mitral valve. (B) CMR showing coronal oblique view of the left ventricular outflow with a dilated aortic root (max. 49
mm at the sinuses), efacement of the sinotubular junction and a dilated proximal ascending aorta. (C) A right ventricular
(RV) transverse stack showing a normal RV and right atrium, with a normal LV size, sigmoid septum and artifact from the
mitral valve prosthesis and minimal artifact from the spinal rods. (D) MRI of thoracic spine showing an incidental finding of
a thoracic cord syrinx.
A
B
C
D

















