
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 4, July/August 2016
264
AFRICA
The Cobas Integra 400 (Roche
®
Clinical System, Roche
Diagnostics, Indianapolis, IN) was used to assess the quantitative
aspectof totalcholesterol(TC),high-densitylipoproteincholesterol
(HDL-C), triglycerides (TG), gamma-glutamyltransferase (GGT),
creatinine and high-sensitivity C-reactive protein (hsCRP) levels in
the serum samples, and glucose levels in fluoride plasma samples.
Glycosylated haemoglobin (HbA
1c
) levels were determined from
EDTA whole blood with ion-exchange high-performance liquid
chromatography (D-10 haemoglobin testing system, Bio-Rad
#220-0101).
The Friedewald formula was used to calculate the quantitative
aspect of low-density lipoprotein cholesterol (LDL-C).
23
The
estimated creatinine clearance (CrCl) rate was calculated with
the Cockcroft–Gault formula.
24
We determined serum interleukin-6 (IL-6) levels with an
electro-chemiluminescence immunoassay (Cobas e411 analyzer,
Roche, Basel, Switzerland). Serum intercellular adhesion molecule
1 (sICAM-1) and vascular cell adhesion molecule 1 (sVCAM-
1) concentrations were assessed by sandwich ELISAs (human
sICAM-1 and human sVCAM-1 assay, IBL, Hamburg, Germany).
Statistical analysis
Statistical analyses were performed using Statistica
®
12 (StatSoft,
Inc, Tulsa, OK, USA). Descriptive statistics, including the
mean and standard deviation, were performed on data with a
normal distribution. If not normally distributed, the data were
logarithmically transformed and presented as the geometric
mean and the fifth and 95th percentiles.
We used independent
t
-tests to determine differences between
normotensives and hypertensives or chi-squared tests for
categorical variables. We compared the groups using ANCOVA
while adjusting for age, gender, WC, GGT, tobacco and anti-
hypertensive medication use. We plotted quartiles of cSBP
against carotid features, and compared carotid features using
ANOVA and ANCOVA while adjusting for cSBP.
We used single and linear regression analyses to determine
associations between carotid measures and cardiometabolic
risk factors, health behaviours, inflammation and endothelial
activation. Multiple regression analyses were done to determine
independent associations between the carotid characteristics
and cardiometabolic risk factors, with the dependent variables
including CD and IMT, and CSWA and max LD. The following
co-variates were included in the regression model: locality,
gender, age, WC, cSBP, heart rate, LDL-C, HbA
1c
, CrCl,
hsCRP, ICAM-1, GGT, tobacco use and additionally for the
hypertensive group, anti-hypertensive medication use.
Results
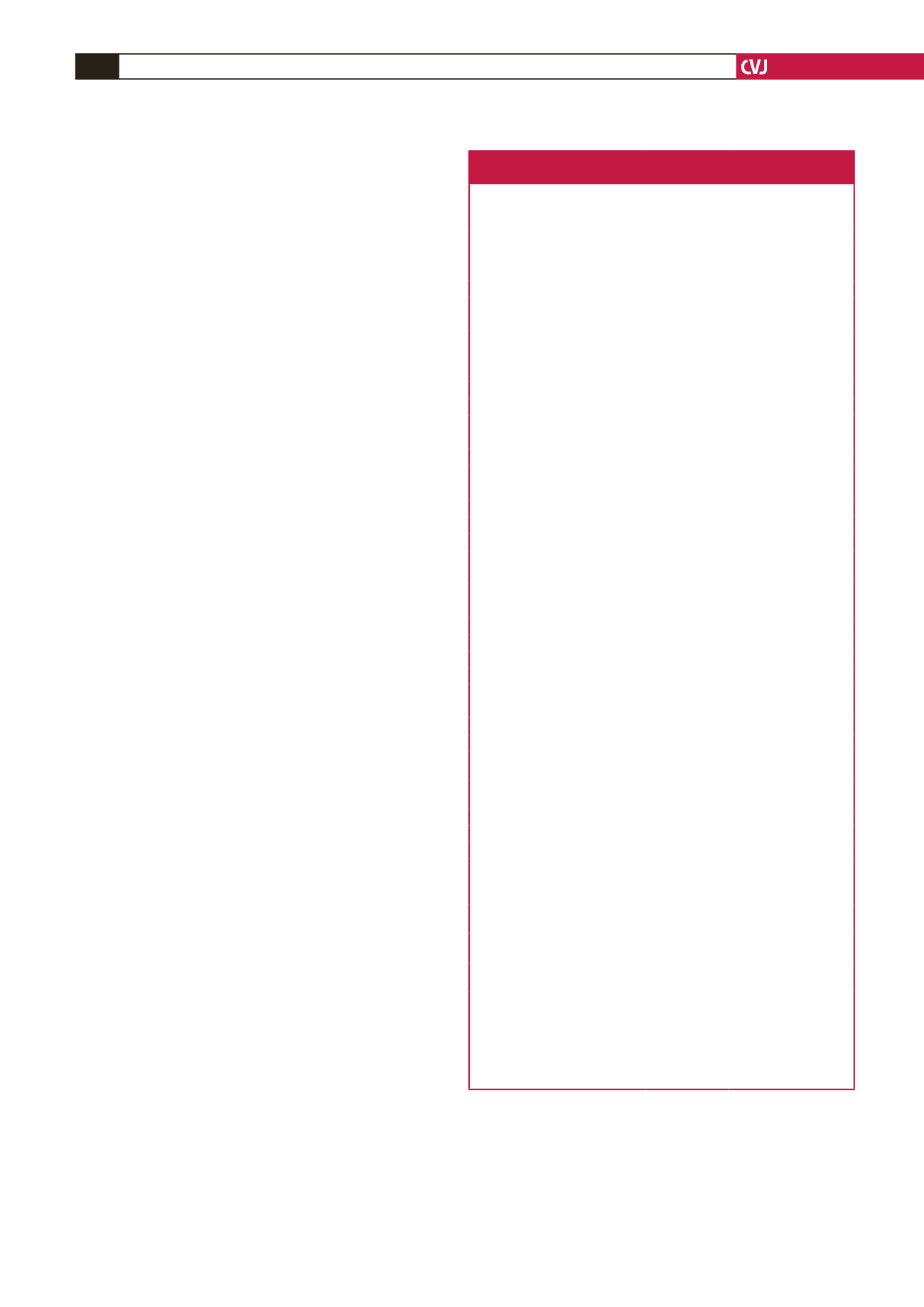
The characteristics of normotensive and hypertensive black
Africans are shown in Table 1. The hypertensives were older,
had a higher BMI and WC, and a larger percentage were from
an urban area than the normotensives. All the cardiovascular
measurements, as well as carotid characteristics, glycaemic and
inflammatory markers, ICAM-1, TG, GGT and self-reported
alcohol use were significantly higher in the hypertensive group.
After adjustments for age, gender, WC, GGT, tobacco
and anti-hypertensive medication use (Table 2), all carotid
characteristics except IMT remained significantly different.
The inflammatory and glycaemic markers, lipids and adhesion
molecules did not differ however after the above adjustments.
The carotid characteristics plotted against quartiles of
cSBP are shown in Fig. 2. All the carotid characteristics
changed significantly with increasing cSBP before and after the
adjustments.
Table 1. Characteristics of normotensive and
hypertensive black Africans
Normotensive
(
n
=
241)
Hypertensive
(
n
=
351)
p
-value
Men,
n
(%)
90 (37.3)
129 (36.8)
0.88
Urban,
n
(%)
78 (32.4)
178 (50.7)
<
0.001
Age, years
52.8
±
8.93
59.0
±
10.0
<
0.001
Anthropometry
Waist circumference, cm
78.7
±
11.9
84.7
±
13.5
<
0.001
Body mass index, kg/m
2
24.7
±
6.87
26.6
±
7.85
0.003
Cardiovascular measures
Brachial SBP, mm Hg
119
±
11.9
157
±
22.4
<
0.001
Brachial DBP, mm Hg
78.9
±
7.23
100
±
12.5
<
0.001
Heart rate, bpm
61.8
±
14.7
67.8
±
17.9
<
0.001
Central SBP, mm Hg
116
±
12.8
150
±
22.2
<
0.001
Central PP, mm Hg
37.4
±
11.8
50.9
±
20.4
<
0.001
Carotid dorsalis pedis PWV, m/s
8.25
±
1.35
10.0
±
1.89
<
0.001
Carotid characteristics
Distensibility
×
10
-3
, 1/kPa
4.72
±
2.00
3.02
±
1.83
<
0.001
Young’s elastic modulus
×
10
3
, kPa 2.17
±
1.07
3.72
±
2.20
<
0.001
Beta-stiffness index
7.10
±
2.62
9.37
±
4.51
<
0.001
Intima–media thickness
,
mm
0.68
±
0.13
0.77
±
0.17
<
0.001
Cross-sectional wall area, mm
2
14.2
±
4.41
17.4
±
5.30
<
0.001
Lumen diameter maximum, mm 6.18
±
0.77
6.60
±
0.85
<
0.001
Lumen diameter minimum, mm 5.74
±
0.72
6.22
±
0.83
<
0.001
Lipids
HDL-C, mmol/l
1.45
±
0.65
1.51
±
0.60
0.30
LDL-C, mmol/l
2.86
±
1.17
2.96
±
1.14
0.29
Triglycerides, mmol/l
1.09 (0.57–2.11) 1.20 (0.59–2.89)
0.039
Glycaemia
Glucose, mmol/l
4.86 (3.91–6.06) 5.27 (3.96–7.90)
<
0.001
HbA
1c
(%)
5.94 (5.30–6.80) 6.08 (5.20–7.80)
0.038
Inflammatory markers
Interleukin-6, pg/ml
3.39 (0.75–23.5) 4.43 (0.75–20.0)
<
0.001
C-reactive protein, mg/l
2.96 (0.21–32.6) 3.84 (0.38–28.4)
0.022
Adhesion molecules
Intercellular adhesion molecule-1,
pg/ml
286
±
92.7
321
±
111
<
0.001
Vascular adhesion molecule-1,
pg/ml
732 (442–1388) 762 (443–1735)
0.23
Renal function
Creatinine clearance, ml/min
91.4 (53.7–163) 91.6 (47.7–164)
0.94
Health behaviours
γ
-glutamyl transferase, U/l
33.7 (11.9–167) 52.7 (13.6–347)
<
0.001
Self-reported alcohol intake,
n
,
total (%)
60/220 (27.3)
159/336 (47.3)
<
0.001
Self-reported tobacco use,
n
,
total (%)
117/229 (51.1)
159/341 (46.6)
0.56
Anti-hypertension medication,
n
,
total (%)
–
124/351 (35.3)
Lipid-lowering medication,
n
,
total (%)
–
5/351 (1.42)
Anti-inflammatory medication,
n
,
total (%)
–
21/351 (5.98)
Data are arithmetic means
±
SD or geometric mean (fifth and 95th percentile
intervals) for logarithmically transformed.
n
, number of participants; SBP, systolic blood pressure; DBP, diastolic blood pres-
sure; PP, pulse pressure; PWV, pulse wave velocity; HDL-C, high-density lipopro-
tein; LDL-C, low-density lipoprotein; HbA
1c
, glycated haemoglobin.

















