
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 27, No 4, July/August 2016
270
AFRICA
Cardio News
Frontline initiatives in early myocardial reperfusion with
ST-elevation myocardial infarction
Concern has been expressed by leading
cardiologists in Africa about the lack
of preparedness of healthcare services
on this continent in relation to the
management of non-communicable
diseases and, specifically, cardiovascular
disease.
1
This may be attributable to a
paucity of surveillance data and registries,
a shortage of physicians and cardiologists,
interventional measures not being in
place, inadequate diagnostic capabilities,
and misguided opinions, as reported.
2
From the South African 2011 census,
3
we know that low household income
compounds the problem of inadequate
healthcare provision, and also lack of
transport to facilities where optimal care
can be provided timeously. Public sector
clinic services are utilised by 61.2% of
households, public hospitals by 9.5%, and
private hospitals, private clinics and other
services by only about 5% of households.
A disparity is evident between the health
facility used and the population group,
in that 17% of black South Africans
versus 88% of white and 64% of Indian
households visit private health facilities.
The Government report explains the
preference for private health institutions
by long waiting times and unavailability
of drugs in the public healthcare system.
However, of the total population, 41%
would be able to reach the health facility
normally used within 30 minutes, and
an additional 17% within 90 minutes.
Disparity is also observed among
population groups concerning coverage
by medical aid or medical benefit schemes
and other private health insurance.
The most recent report from a study
performed at a public academic hospital
in Pretoria in 2015 states that ‘Only 37%
of patients received fibrinolytic therapy
and only 3% received the medication
within one hour’.
4
Similarly, 44.7% of
ST-elevation myocardial infarction
(STEMI) cases reportedly received
fibinolytic therapy at the Groote Schuur
Hospital in Cape Town (2012),
5
and 36%
of South African STEMI cases captured
in the ACCESS registry (2007–2008)
received fibrinolytic therapy.
6
Baseline data for the STEMI Early
Reperfusion Project, undertaken in private
hospitals in the Tshwane metropolis (May
– October 2012) to establish time intervals
along the referral pathways from onset
of symptoms to percutaneous coronary
intervention (PCI), showed that system
delays were evident with inter-facility
transport (IFT) compared with direct
access (DA) to a PCI facility (median
3.7 vs 30.4 hours;
p
< 0.001). Door-
to-balloon times of ≤ 90 minutes were
achieved in a mere 22% of DA and 33%
of IFT patients, and fibrinolysis within
≤ 30 minutes was only achieved in 50% of
DA and 20% of IFT patients.
7
The South African Heart Association
EarlyReperfusion Project for ST-elevation
myocardial infarction commenced in 2012
as an initiative of the South African Heart
Association (SAHA), with Dr Adriaan
Snyders as president of the association.
The pilot study in the Tshwane metropolis
private sector
7
informed an observational
multi-centre study in South African
hospitals, launched in the last quarter of
2015, to identify factors that contribute
to delays in early reperfusion for STEMI.
A sub-study will be launched in 2017 to
investigate whether implementation of
a hub-and-spokes model (hub hospitals:
PCI-capable hospitals, and spokes: referral
hospitals), with the application of an ICT
(an ECG-capturing, patient-monitoring,
communication and data-capturing
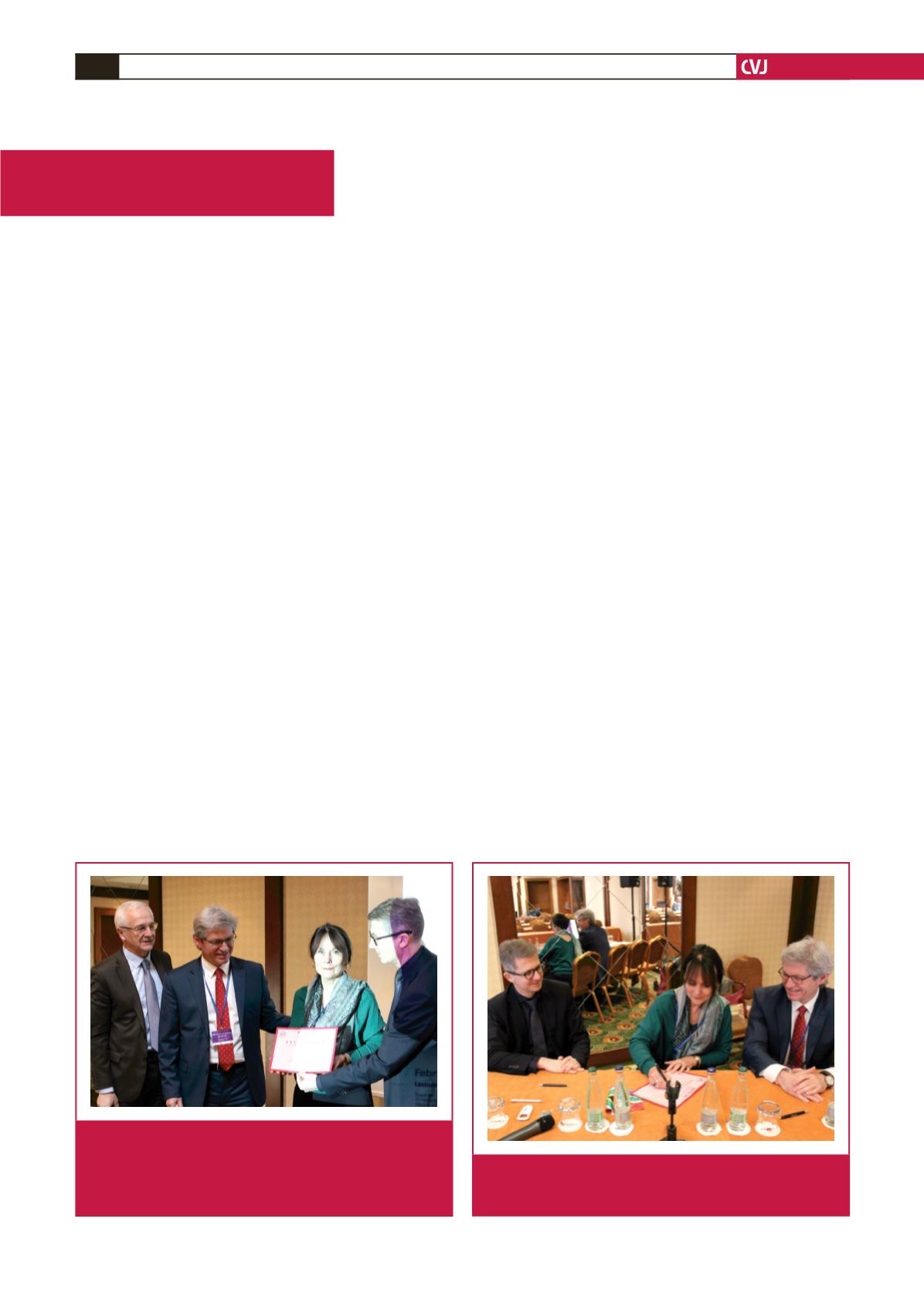
Declaration of intent to fulfil the Stent-for Life mission in
South Africa. From left to right: Dr William Wijns (SFL initiative
founder and past president of EAPCI), Prof Petr Kala (SFL
chairman), Prof Rhena Delport (SFL South Africa) and Prof
Stephan Windecker (president of EAPCI).
Signing the intent. From left to right: Prof Stephan Windecker
(president of EAPCI), Prof Rhena Delport (SFL South Africa)
and Prof Petr Kala (SFL chairman).

















