
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 4, July/August 2017
AFRICA
255
general hospital to which referrals can be made, while each
general hospital or secondary centre should be attached to a
tertiary centre or teaching hospital. Furthermore, there should
be annual reports for each primary and comprehensive health
centre, and performance should be rewarded.
Finally, governments should take the lead and involve the
private sector, non-governmental organisations and academia.
Such projects require constant funding and support.
Conclusion
The high burden of CVD and diabetes mellitus in sub-Saharan
Africa means that individual governments must develop strategic
plans to equip their primary care clinics with well-trained
non-physician healthcare workers and basic instruments, such
as blood pressure apparatus, kits for urinalysis, and blood
glucose and cholesterol checks if an epidemic of chronic
non-communicable diseases is to be averted on the sub-continent.
Governments should also set up a referral system whereby there
is supervision and referral from primary care to secondary
centres, and two to five primary care centres should be attached
to a secondary centre.
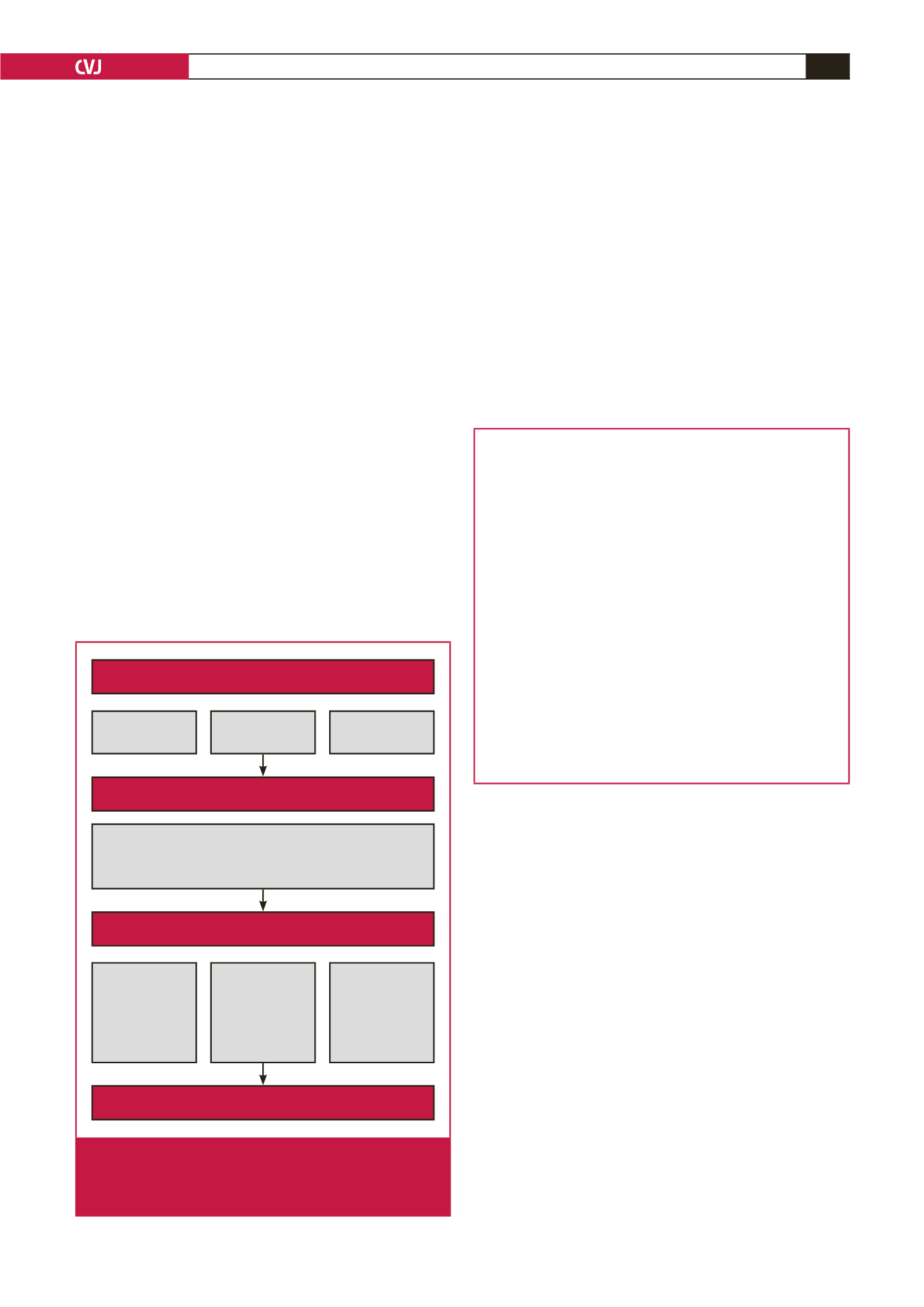
The Seychelles experience shows that the key drivers of
effective primary care to yield population-level impacts on
diabetes mellitus and CVD include research, a non-physician-
based approach, and integration of the media, the general
population, academia and non-governmental organisations. For
such a programme to succeed there must be a holistic framework,
developed by the government and coordinated by the NCD unit
of the federal ministry of health, as shown in Fig. 1. It should
involve research on CVD and diabetes, structured training of
non-physician healthcare workers, appropriate equipping of
primary healthcare centres and correct referral systems from
primary to secondary centres.
Limited resources were a disadvantage in the Seychelles
programme and would also be in sub-Saharan Africa. This
could be overcome with the support of non-governmental
agencies and the private sector, however, they would invest in
such programmes only if they had confidence in the government
of the country.
Key points
•
CVD plays a leading role in the disease spectrum of sub-
Saharan Africa, with stroke and ischaemic heart disease
ranked as seventh and 14th leading causes of death,
respectively, on this sub-continent.
•
Limited resources and the high cost of CVD treatment
necessitate that primary prevention should have a high
priority for CVD control in sub-Saharan Africa.
•
For any CVD intervention programme to succeed on the
sub-continent, a community-orientated approach must
be taken, especially in rural areas where transportation
is difficult, deterring people from seeking medical help at
urban and semi-urban health facilities.
•
Primary health centres therefore need to be equipped
with trained non-physician personnel who are supervised
by physicians, and also with basic tools such as blood
pressure apparatus, glucometers, urinalysis strips and
point-of-care machines for cholesterol checks.
This project was supported by award number D43TW008330 from the
Fogarty International Centre. The content is solely the responsibility of
the authors and does not necessarily represent the official view of the
Fogarty International Centre or the National Institute of Health. Dr
Dike Ojji is currently a Research Fellow at the Soweto Cardiovascular
Research Unit, University of Witwatersrand, South Africa under the Wits
Non-Communicable Disease Research Leadership Programme, funded by
the NIH (Fogarty) training programme. Dr Kim Lamont was funded by the
NRF scarce skills award.
References
1.
Murray CJL, Global Burden of Disease study group 2010. Disability-
adjusted life years (DALYS) for 291 diseases and injuries in 21 regions,
1990–2010: a systematic analysis for the Global Burden of Disease study
2010.
Lancet
2012;
380
: 2197–2223.
2.
Mathers CD, Loncar D. Projections of global mortality and burden of
disease from 2002 to 2030.
PLoS Med
2006;
3
(11); e442.
3.
Opie LH, Mayosi BM. Cardiovascular disease in sub-Saharan Africa.
Circulation
2005;
112
: 3536–3540.
4.
Expert Committee on Prevention of Coronary Heart Disease. WHO
Technical Report Series No 678. World Health Organization, Geneva,
1982.
Functional organisation of PHC services
Prerequisite
Enabling work environment and proper supervision
Supermarket
approach
• The size and structural set up of the clinic
• The availability and competency of nurses
• Availibity of equipment and space
PHC team
PARC:
P
roductivity,
A
vailability,
R
esponsibility,
C
ompetence
Comprehensive
healthcare
Organisational
support
SITE:
S
pace,
I
nfastructure,
T
ransport,
E
quipment
One-stop shop
Collaboration
PHC team,
C
ommunity,
NGOs,
Academia
Determinants
Fig. 1.
Organisational structure showing how primary health-
care can be effective in preventing cardiovascular
disease. PHC = primary healthcare. NGOs = non-
governmental organisations.

















