
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 28, No 6, November/December 2017
AFRICA
387
Discussion
In this study, we investigated the association between CorT and
PCT. Our results reveal that PCT, MPV, P-LCR, NLR and PLR
of patients with CorT were higher than those of the control
group consisting of patients with a normal coronary artery. Age,
hypertension, diabetes mellitus and PCT were independently
associated with CorT.
CorT is a common coronary angiographic finding. In the
study by Li,
et al
., the prevalence of CorT was 39.1% in patients
with stable angina pectoris.
3
To date the aetiology of CorT is
unclear. There are several possible mechanisms implicated in the
development of CorT. Some authors claim that degeneration
of the elastin layer of the vessel may be the cause of coronary
tortuosity.
11
CorT may be associated with age, hypertension
and atherosclerosis.
12-14
In our study, CorT was independently
associated with hypertension, diabetes mellitus, age and PCT.
Li
et al
.
3
found that CorT was positively correlated with
essential hypertension. They hypothesised that the arteries may
become tortuous due to reduced axial strain and hypertensive
pressure in an elastic cylindrical arterial model. Therefore CorT
may be one of the forms of artery remodelling induced by
hypertension due to increased coronary pressure and blood flow.
This is consistent with the findings of our study. We found
a highly significant difference between the CorT and non-CorT
groups regarding the presence of hypertension. However, some
authors suggest that CorT is a common finding seen with aging
and hypertension due to elongation and dilatation of the arteries
associated with left ventricular hypertrophy.
13,15
CorT may be related to typical anginal pain with angiographic
evidence of objective ischaemia without significant coronary
lesions. This could be due to compression of the vessel during
heart contraction.
14
CorT has a minor influence on coronary blood
supply at rest, whereas during exercise, patients with CorT may
lack the ability to adjust distal resistance sufficiently to compensate
for the extra resistances generated by tortuosity, and this may
further lead to an ineffective regulation of the blood supply.
16
Li
et al.
17
found that CorT can result in decreased coronary
blood pressure depending on the severity of tortuosity, and
therefore severe CorT may cause myocardial ischaemia. In
another study, Li
et al.
5
found that CorT was associated with
reversible myocardial perfusion defects in patients with chronic
stable angina and normal coronary angiograms.
CorT is associated with coronary atherosclerotic changes
regardless of the presence of actual coronary stenosis. CorT may
induce subclinical atherosclerosis in the absence of significant
obstructive lesions.
18
Severe tortuosity in the coronary arteries
simplifies atherosclerosis.
19
Therefore atherosclerosis is more
common in patients with coronary artery tortuosity, as greater
curvature has more areas of low-shear wall stress. Shear stress is
an essential causal factor in the development of atherosclerosis
20
and in vulnerable plaque rupture.
21
Davutoglu
et al
.
22
found that
CorT was strongly associated with subclinical atherosclerosis
indicated by carotid intima–media thickness and retinal artery
tortuosity.
On the other hand, some studies found that CorT was
negatively correlated with significant coronary artery disease
detected by coronary angiography.
3,23
Esfahani
et al
.
24
showed that
the mean Gensini index of the tortuous group was significantly
lower than that of the non-tortuous group.
Platelet activation plays a significant role in the initiation
and progression of atherosclerosis.
25,26
Platelets release many
mediators such as thromboxanes, and interleukin (IL)-1, IL-3
and IL-6 that may lead to increased inflammation.
27
PCT is part of the routine CBC haematology and provides
more comprehensive data about total platelet mass because
the PCT is the product of the platelet count and the MPV.
28
Ekici
et al
.
29
reported a strong association between MPV and
angiographic severity of coronary artery disease. Several studies
have shown that there was a strong relationship between PCT
and saphenous vein disease and slow coronary flow.
30,31
The
association between haematological parameters and adverse
cardiovascular outcomes has been shown in previous studies.
32-35
In this study, we found that PCT, MPV, NLR and PLR of the
CorT group were significantly higher than those of the control
group. Hypertension, diabetes mellitus, age and PCT were
independently associated with CorT.
Our study has some limitations. First was the small sample
size. Second, coronary angiography, which we used, only shows
the arterial lumen, whereas cardiac computed tomography
(CT) angiography and intravascular ultrasound (IVUS) allow
visualisation of the lumen as well as the vascular wall. Cardiac
CT and IVUS allow detection and characterisation of coronary
atherosclerotic plaques. Accordingly, cardiac CT helps in the
evaluation of atherosclerotic plaques that are undetected by
conventional coronary angiography.
Conclusions
This is the first study to evaluate the relationship between CorT
and PCT. Hypertension, diabetes mellitus, age and PCT were
independently associated with CorT. We concluded that CorT is
associated with increased pro-inflammatory processes related to
coronary artery disease. Long-term follow up of PCT levels in
patients with CorT with regard to the development of coronary
artery disease may be useful.
References
1.
Turgut O, Yilmaz A, Yalta K, Yilmaz BM, Ozyol A, Kendirlioglu O,
et al
. Tortuosity of coronary arteries: an indicator for impaired left
ventricular relaxation?
Int J Cardiovasc Imaging
2007;
23
: 671–677.
2.
Han HC. Twisted blood vessels: symptoms, etiology and biomechanical
mechanisms.
J Vasc Res
2012;
49
: 185–197.
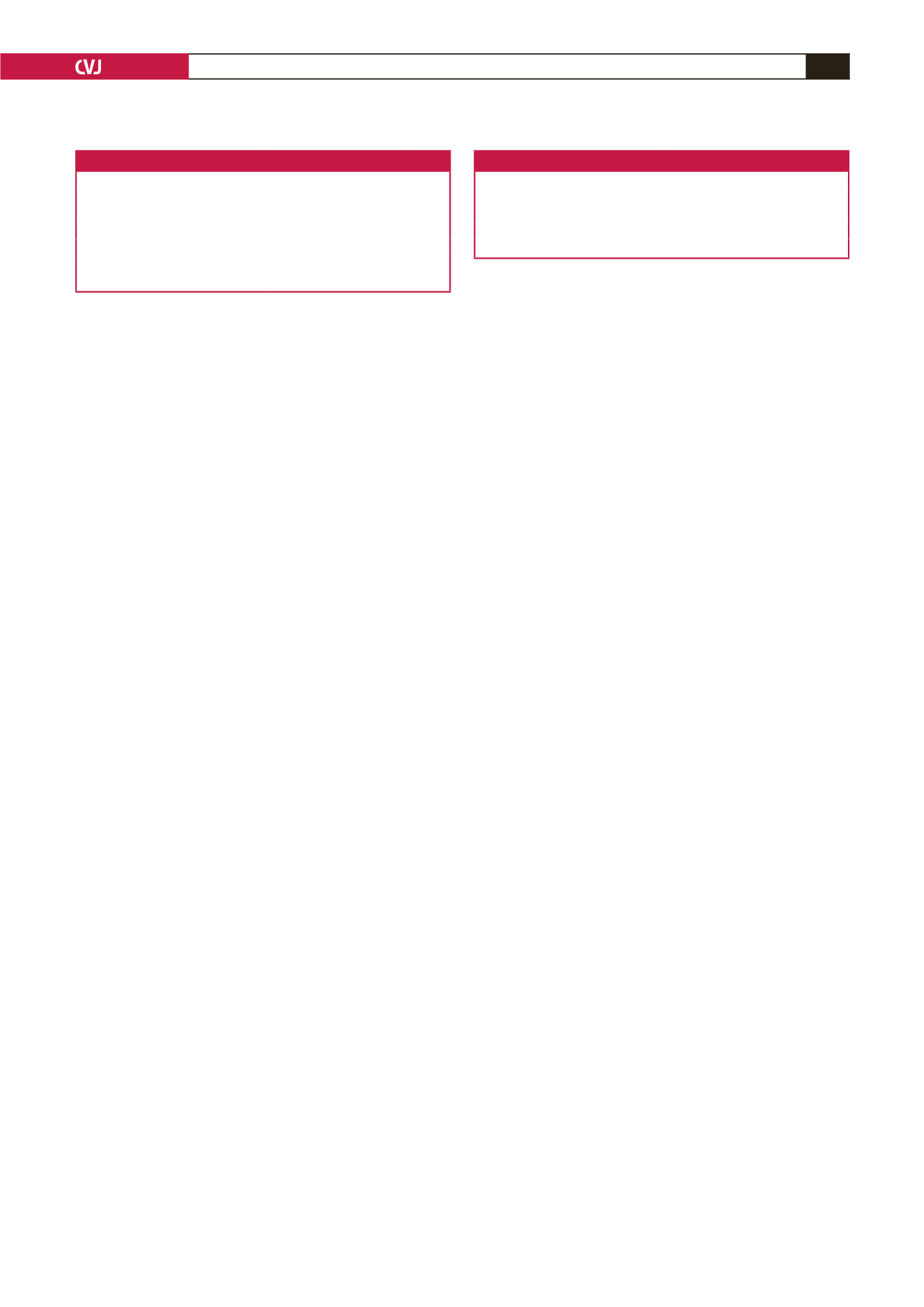
Table 3. Univariate analysis of predictors for coronary tortuosity
Predictor variables
OR (95% CI)
p
-value
Age, years
3.275 (1.943–5.627)
<
0.001
Diabetes mellitus,
n
(%)
2.539 (1.675–3.592)
<
0.001
Hypertension,
n
(%)
2.856 (1.345–3.863)
<
0.001
Female gender,
n
(%)
2.348 (1.857–4.362)
<
0.001
Plateletcrit
2.896 (1.964–4.857)
<
0.001
Neutrophil:lymphocyte ratio
1.854 (1.376–2.827)
0.001
Table 4. Multivariate analysis of predictors for coronary tortuosity
Predictor variables
OR (95% CI)
p
-value
Age, years
1.826 (1.354–2.167)
<
0.001
Hypertension,
n
(%)
2.158 (1.462–2.937)
<
0.001
Diabetes mellitus,
n
(%)
1.583 (1.362–2.835)
<
0.001
Plateletcrit
1.634 (1.345–2.724)
<
0.001

















