
CARDIOVASCULAR JOURNAL OF AFRICA • Volume 31, No 5, September/October 2020
276
AFRICA
ST-segment depression > 0.3 mV with giant inverted T waves
in leads V
3
–V
6
(Fig. 1A). An emergency blood test showed a
white blood cell (WBC) count of 46.38 × 10
9
cells/l, neutrophils
of 17.3% and eosinophils of 73.7%, and a total blood count of
34.18 × 10
9
cells/l. The platelets, red blood cells and haemoglobin
were in the normal range. Levels of troponin-I, aspartate
aminotransferase, lactate dehydrogenase, C-reactive protein and
D-dimer were elevated at 2.24 ng/ml, 76 IU/l, 1173 IU/l, 18.3
mg/l and 845 ng/ml, respectively. Levels of myoglobin, creatine
kinase and creatine kinase isoenzyme were normal.
The emergency room doctor suspected the patient of having
acute coronary syndrome such as non-ST-elevation myocardial
infarction, therefore he transferred him for an emergency coronary
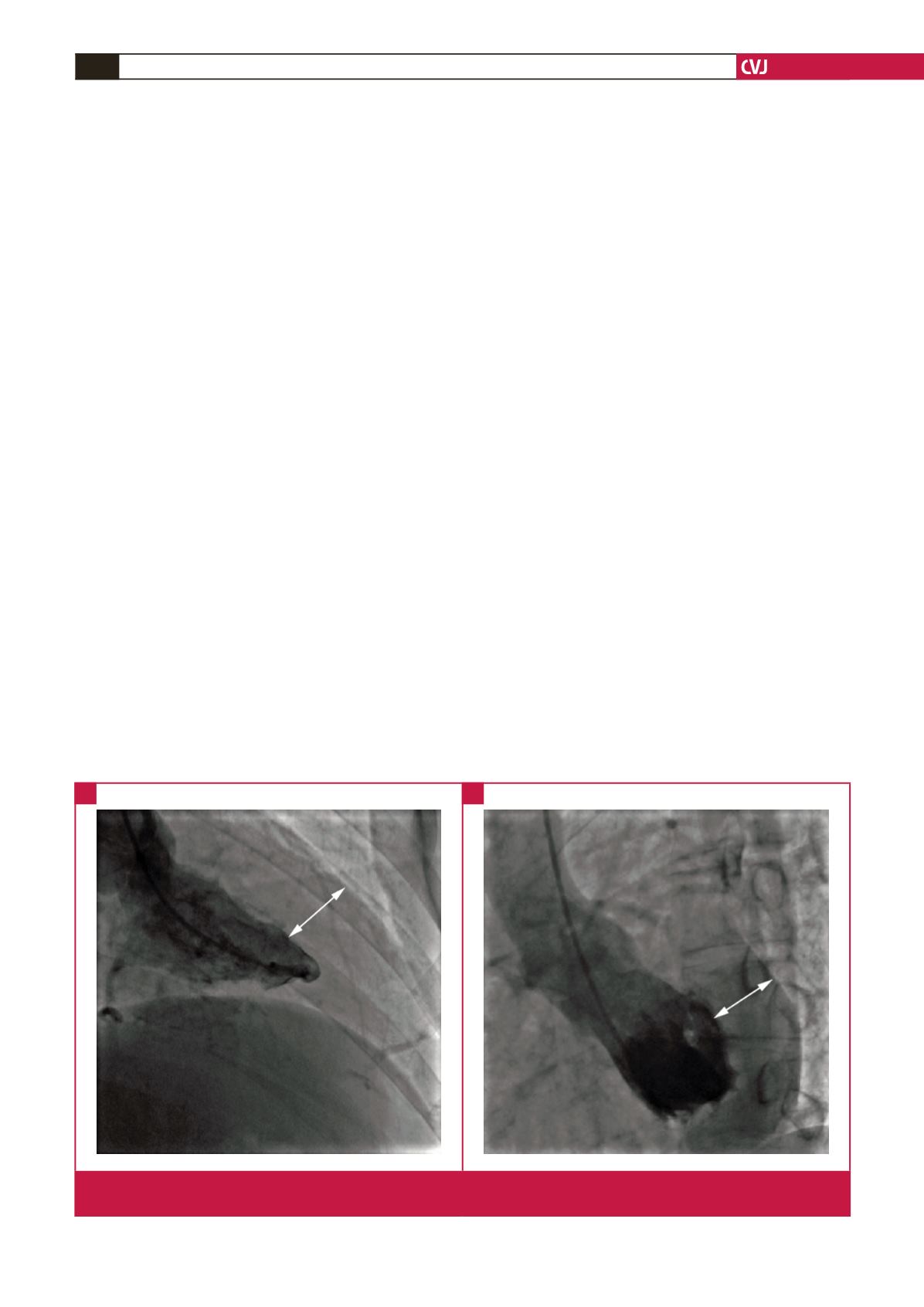
evaluation. The coronary angiogram showed no coronary artery
abnormalities, and the left ventriculography examination revealed
normal myocardial movement associated with a substantial
thickening of the LV endomyocardium (Fig. 2).
A further peripheral blood smear showed 20% neutrophilic
granulocytes and 68% eosinophilic segmented granulocytes. A
bone marrow biopsy indicated that the rates of eosinophilic
myelocytes, eosinophilic metamyelocytes, eosinophilic stab
granulocytes and eosinophilic segmented granulocytes were 0.5,
12.5, 15.5 and 49%, respectively. No abnormalities were found
in glucose, plasma protein, bilirubin, ions, blood lipids, NT-pro
brain natriuretic peptide (NT-proBNP) and vitamin B
12
levels,
and renal and coagulation function.
His urine and stool tests were normal. The antibodies to
hepatitis B and C viruses,
Treponema pallidum
and human
immunodeficiency viruswere negative. Therewere noabnormalities
in the tuberculin test, thyroid function, rheumatic, immune and
tumour biomarkers, and no parasites were found. Allergen tests
showed IgE > 200 IU/ml with short ragweed and artemisia at
2.12 IU/ml, and cashew, peanut and soybean at 3.70 IU/ml.
His chromosome pattern was 46, XY [20] with no positivity in
fusion genes, including
PDGFR
α
(
FIPIL1/PDGFR
α
),
PDGFR
β
,
FGFRI
,
AMLI
,
CAN
,
MLL
,
BLR/ABL
and
JAK2
.
Two-dimensional transthoracic echocardiography (TTE)
performed the day after admission revealed a markedly thickened
LV wall accompanied by mild mitral regurgitation of 2.5 cm
2
(Fig.
3A). The sizes of the bilateral atrial and ventricular chambers were
normal with no evidence of pericardial effusion. The LV systolic
function was normal with an ejection fraction (EF) of 67%, but a
mild LV diastolic dysfunction was noted with E (0.52 m/s)/A (0.77
m/s) = 0.67, e
′
(6.7 cm/s)/a
′
(8.5 cm/s) = 0.78, and E/e
′
= 7.76.
Chest computed tomography (CT) showed increased
bronchovascular shadows at the bilateral lung bases (Fig. 4A).
Abdominal ultrasound showed no abnormalities in the liver,
spleen, gall bladder, pancreas, kidneys and adrenal glands. Cine-
cardiac magnetic resonance (CMR) imaging (Skyra 3.0 T scanner,
Siemens, Munich, Germany) with steady-state free precession
(True FISP) sequences revealed a substantially thickened LV
endomyocardium and low-density thrombotic signals within the
LV cavity (Fig. 5). CMR parameters of cardiac function were
EF of 50%, LV end-diastolic volume of 149 ml, LV end-systolic
volume of 75 ml, stroke volume of 74 ml, cardiac output of 4.5
l/min and cardiac index of 2.3 l/min/m
2
.
Secondary hypereosinophilia due to drugs, allergic and
connective tissue disorders, parasites, malignancies, rheumatism,
as well as haematological neoplasm with clonal eosinophilia was
excluded. The patient was diagnosed as IHES and IHES-related
cardiac injuries.
The patient received subcutaneous injections of low-molecular
weight heparin of 40 mg twice daily for five consecutive days,
and oral warfarin and prednisolone at an initial dose of 2.5 and
75 mg/day, respectively. Seven days after hospital admission, the
patient’s symptoms completely resolved and the eosinophil count
dropped significantly. Repeat ECG showed similar changes to
those before admission, whereas TTE recheck showed a normal
Fig. 2.
Left ventriculography at the ventricular end-systolic phase. A: right anterior oblique 30° view. B: left anterior oblique 60° view.
The white double arrows indicate the substantially thickened endomyocardium of the LV.
A
B



















